-
 Cancer
CancerIncreased detection of low-risk tumors driving up thyroid cancer rates
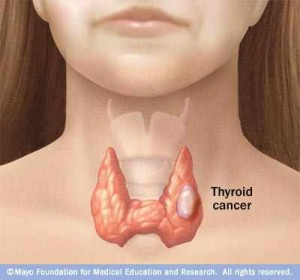 ROCHESTER, Minn. — Low-risk cancers that do not have any symptoms and presumably will not cause problems in the future are responsible for the rapid increase in the number of new cases of thyroid cancer diagnosed over the past decade, according to a Mayo Clinic study published in the journal Thyroid. According to the study authors, nearly one-third of these recent cases were diagnosed when clinicians used high-tech imaging even when no symptoms of thyroid disease were present.
ROCHESTER, Minn. — Low-risk cancers that do not have any symptoms and presumably will not cause problems in the future are responsible for the rapid increase in the number of new cases of thyroid cancer diagnosed over the past decade, according to a Mayo Clinic study published in the journal Thyroid. According to the study authors, nearly one-third of these recent cases were diagnosed when clinicians used high-tech imaging even when no symptoms of thyroid disease were present.
“We are spotting more cancers, but they are cancers that are not likely to cause harm,” says the study's lead author, Juan Brito Campana, M.B.B.S., an assistant professor of medicine at Mayo Clinic. “Their treatment, however, is likely to cause harm, as most thyroid cancers are treated by surgically removing all or part of the thyroid gland. This is a risky procedure that can damage a patient’s vocal cords or leave them with lifelong calcium deficiencies.”
MEDIA CONTACT: Joe Dangor, Mayo Clinic Public Affairs, 507-284-5005, newsbureau@mayo.edu
Dr. Brito says harm is not limited to physical suffering. “Treatment can cause financial hardship for patients and their families and for society as a whole, as millions of dollars are spent for unnecessary and problematic surgeries,” he says.
According to Dr. Brito, the aggregate national cost these procedures in the U.S. was $1.6 billion in 2013 and likely will exceed $3.5 billion by 2030. At the same time, the incidence of thyroid cancer is increasing more rapidly than that of any other cancer and is on track to become the third most common cancer in women.
In this study, Dr. Brito and his colleagues drew on data from the Rochester Epidemiology Project. They analyzed the records of 566 men and women who were diagnosed with thyroid cancer in Olmsted County, Minnesota, between 1935 and 2012. Specifically, they examined the number of new cases of thyroid cancer, the deaths due to the disease, and the method of diagnosis.
Researchers found that the number of new cases of thyroid cancer doubled in recent years – from 7.1 per 100,000 people from 1990 to 1999 to 13.7 per 100,000 people from 2000 to 2012. Over the same period, the number of new patients with thyroid cancer presenting with symptoms of thyroid cancer remained the same. In contrast, the number of new cases of silent thyroid cancer – the kind where patients have no symptoms – almost quadrupled. The proportion of patients with thyroid cancer who die of the disease has not changed since 1935.
The study found that the most frequent reasons for identifying silent thyroid cancer were review of thyroid tissue removed for benign conditions (14 percent); incidental discovery during an imaging test (19 percent); and investigations of patients with symptoms or palpable nodules that were clearly not associated with thyroid cancer, but triggered the use of imaging tests of the neck (27 percent).
“We are facing an epidemic of diagnosis in thyroid cancer,” says Dr. Brito. “Now that we know where all these new cases are coming from, we can design strategies to identify patients with thyroid cancer who can benefit from our treatment without condemning other patients to unnecessary tests, treatment, suffering, and costs.”
Researchers say one approach to curtail the detection of these lesions would be to limit the use of certain imaging technologies. Another tactic would be to engage patients in deliberating their treatment options. In many cases, active surveillance may be preferred over surgery by patients with small, relatively benign cancers that could take decades to grow to any appreciable size or cause life-threatening problems.
Dr. Brito thinks something as simple as not using the word “cancer” to refer to these small and silent thyroid lesions could reduce the number of unnecessary treatments for patients with a more favorable prognosis. Rather than calling these lesions thyroid cancer, he would recommend a less emotionally charged term, such as papillary lesions of indolent course.
Co-authors include Alaa Al Nofal, M.D., Victor Montori, M.D., Ian Hay, M.D., Ph.D., and John Morris III, M.D. – all of Mayo Clinic.
The study was made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health (R01AG034676).
###
About Mayo Clinic
Mayo Clinic is a nonprofit worldwide leader in medical care, research and education for people from all walks of life. For more information, visit http://www.mayoclinic.org and http://www.mayoclinic.org/news.







