-
Cancer
Surgery Proving Option for More Pancreatic Cancer Patients
November is Pancreatic Cancer Awareness Month
Pancreatic cancer has long proved the least survivable of the most common forms of cancer, in part because it tends to spread before symptoms appear. Surgery has offered the longest remissions, but for many people with advanced cancer, an operation wasn’t an option. Now, thanks to improvements in chemotherapy, radiation and surgery, even this most recalcitrant of cancers is starting to budge, says Mark Truty, M.D., a Mayo Clinic gastrointestinal surgeon.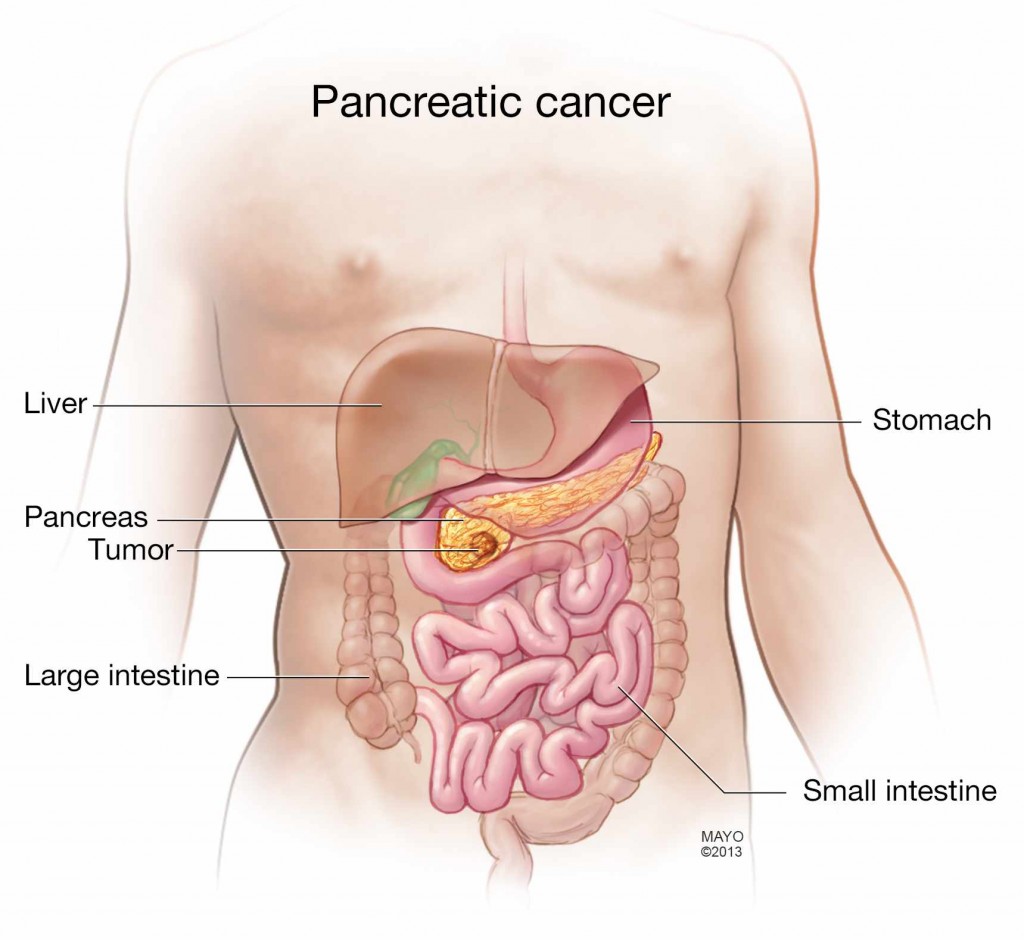
Dr. Truty and his colleagues are now performing complex tumor removal operations on pancreatic cancer patients who in the past would have been considered inoperable — and they are seeing survival times rise significantly.
“We know that patients who go through our preoperative protocol and to the operating room do significantly better than average, compared to historical outcomes. We’re looking at three- to four-fold improvement in overall survival,” Dr. Truty says. “In the past few years, we have done operations that were never performed before. With improved chemotherapy and radiation therapy, we’re now beginning to push the envelope surgically.”
Journalists: Video and audio cuts of Dr. Truty are available in the downloads.
For interviews with Dr. Truty, please contact Sharon Theimer in Mayo Clinic Public Affairs at 507-284-5005 or newsbureau@mayo.edu.
Dr. Truty explains who is a candidate for pancreatic cancer surgery, the types of operations, recovery times and outcomes:
Who is a candidate for pancreatic cancer surgery?
About 50,000 people are diagnosed with pancreatic cancer each year in the U.S, and in about half, the cancer has spread to other parts of their bodies, ruling out surgery, Dr. Truty says. Historically, only about 7 percent of pancreatic cancer patients have lived at least five years after diagnosis.
In roughly 15 percent of patients, the cancer is isolated within the pancreas, making them clear candidates for tumor removal surgery, he says.
In the other 35 percent, the cancer has grown outside the pancreas to involve critical blood vessels, but not yet spread to other parts of the body. Those patients too were told in the past that surgery wasn’t an option, but increasingly it is, Dr. Truty says.
Whether such patients are surgical candidates is assessed case by case. They first receive chemotherapy and radiation therapy, and their health care team works with them to improve their diet and overall physical condition, an effort known as prehabilitation, before surgery is considered, Dr. Truty says.
“We then look at the whole picture,” he says. “Not just a CT scan. We look at whether the tumor can be removed and we can achieve a negative margin – no cancer cells left around it. We assess the risk of cancer spreading from surgery, and tumor marker elevation.”
Patients with complex surgeries also work with dieticians and physical therapists after their operations to speed their recoveries, and those who recover well may get more chemotherapy, Dr. Truty says.
What types of surgery are there, and how long does it take to recover?
If the tumor is only in the pancreas, the type of surgery depends on where it is. If it is in the organ’s head or neck, a Whipple procedure, also known as a pancreaticoduodenectomy, removes the head of the pancreas, part of the small intestine and bile duct, and the gallbladder.
If the tumor is in the body or tail of the pancreas, a surgeon will perform a distal pancreatectomy to remove the organ’s body and tail and the spleen. Some cases can now be done laparoscopically, a minimally invasive method that usually means a faster recovery.
Recovery typically includes a week in the hospital and two months recuperating at home.
The more complex surgeries, those in cases previously considered inoperable, sometimes pair a Mayo gastrointestinal surgeon with a vascular surgeon. The operations may involve critical veins, arteries and other organs and require complex reconstructions, including arterial and venous grafts and partial or entire removal of organs. Those patients are in the hospital twice as long as those with simpler surgeries; recovery at home usually takes at least three months, Dr. Truty says.
What is the range of outcomes?
“The problem with pancreas cancer is that unfortunately, the numbers don’t lie. It’s a very bad tumor. It’s the fourth-leading cause of cancer death, and by 2020, it will be the second-leading cause of cancer death, surpassing breast cancer,” Dr. Truty says. “The incidence is slowly rising.”
Under the approach used for decades — for patients with only a tumor in the pancreas, an operation followed by chemotherapy — the average patient lived roughly two years after diagnosis. Those whose cancer spread and was considered inoperable typically lived less than a year after diagnosis.
Now, patients with more advanced cancer who have aggressive chemotherapy, radiation and complex surgery are seeing average survival times of three to four years and counting, Dr. Truty says. He has only been performing the complex surgeries for about four years, so does not yet have statistics beyond that. With the advances in treatment, up to twice as many people may be surgical candidates, he says.
Dr. Truty hopes the improved treatment options begin to counter what he sees as a sense of nihilism among physicians and patients, and that people who are told nothing can be done seek a second opinion. Half of his complex surgery patients were told elsewhere that surgery wasn’t an option.
“I had a personal experience with pancreas cancer in my family: my father. I would have done anything for an additional holiday, another year, another two years, hopefully longer,” Dr. Truty says. “And we’re hoping to offer that to these patients and their families.”
https://vimeo.com/143628556







