-
Featured News
Mayo Clinic Q and A: Understanding myofascial pain syndrome and fibromyalgia
DEAR MAYO CLINIC: What’s the difference between myofascial pain syndrome and fibromyalgia? How are they diagnosed?
ANSWER: Both of the conditions you mention are chronic pain disorders, meaning they cause pain that lasts for long periods of time and can be difficult to manage. Myofascial pain syndrome involves mainly muscular pain; whereas, fibromyalgia includes more widespread body pain, along with other symptoms, such as headaches, bowel problems, fatigue and mood changes.
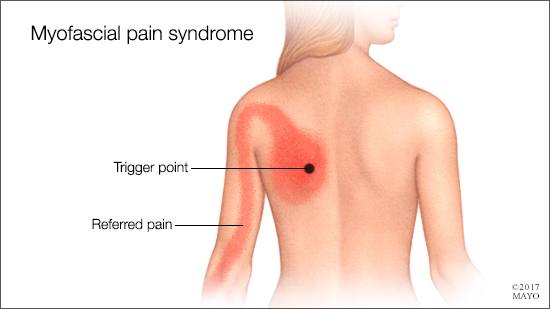
In people with myofascial pain syndrome, sensitive areas of tight fibers form within a muscle or an adjoining muscle group, typically due to muscular injury or overuse. As a result, a tender, painful knot develops in the muscle. When pressure is placed on that area, called a tender point or trigger point, it leads to deep, aching muscle pain.
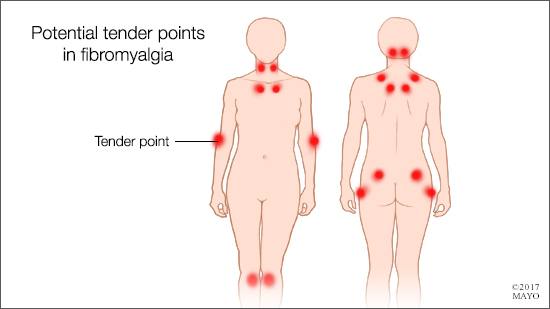
The pain of fibromyalgia is different, because it’s diffuse, migratory and involves both muscles (myalgia) and joints (arthralgia). It affects both sides of the body — above and below the waist. Furthermore, the pain may move — a process called migratory phenomenon — from one part of the body to another over time. The discomfort of fibromyalgia usually is felt as both joint and muscle aches and pain, without any redness or swelling caused by inflammation. Researchers believe that fibromyalgia causes pain because the disorder affects the way the brain processes pain signals, amplifying painful sensations.
Fibromyalgia causes other symptoms beyond pain, too. One of the most common is fatigue. People who have fibromyalgia often wake up in the morning still feeling tired, even when they have slept for long periods of time. Problems with concentration, attention and mental focus also may plague those with fibromyalgia.
There aren’t any specific tests available that can definitively diagnose myofascial pain syndrome or fibromyalgia. Both are diagnosed clinically.
Myofascial pain syndrome often can be identified based on symptoms and a physical examination. During the exam, a health care provider may apply gentle pressure to the painful muscle, feeling for tense areas. Certain ways of pressing on a tender point can elicit specific responses, such as a muscle twitch. Because muscle pain can have many possible causes, additional tests may be recommended to rule out other diseases or conditions before making a diagnosis of myofascial pain syndrome.
Diagnosing fibromyalgia is a two-stage process. First, because many other disorders can mimic the symptoms of fibromyalgia, it’s important that those be ruled out. Blood tests and other diagnostic tests should be performed to confirm that the pain is not the result of another condition, such as arthritis, lupus, a connective tissue disorder or a thyroid disorder.
The second step in fibromyalgia diagnosis is assessing an individual’s symptoms using a tender point count and validated survey criteria, such as the Widespread Pain Index and Symptom Severity Scale. In most cases, if the pain is widespread, has lasted for three months or more, is not associated with an underlying medical condition that could cause the pain, and meets the validated survey criteria, then the diagnosis of fibromyalgia is made.
After diagnosis, it’s usually best for people with these disorders to work with a health care provider who is trained in, and has experience working with, chronic pain conditions. Although no cure is available for myofascial pain syndrome or fibromyalgia, these conditions often can be effectively managed with a personalized treatment plan that minimizes pain, improves overall health and enables an individual to engage in normal routines and activities. — Dr. Arya Mohabbat, General Internal Medicine, Fibromyalgia and Chronic Fatigue Clinic, Mayo Clinic, Rochester, Minnesota







