-
Featured News
Mayo Clinic Q and A: Treatment options for herniated disk
 DEAR MAYO CLINIC: I have a herniated disk in my lower spine that’s causing a lot of pain and leg numbness. For three months, I’ve tried medications and physical therapy, but it’s not helping. My doctor now recommends surgery. She says there’s a way to do it that is less invasive than traditional surgery. How does that work? Is that type of surgery effective for a herniated disk?
DEAR MAYO CLINIC: I have a herniated disk in my lower spine that’s causing a lot of pain and leg numbness. For three months, I’ve tried medications and physical therapy, but it’s not helping. My doctor now recommends surgery. She says there’s a way to do it that is less invasive than traditional surgery. How does that work? Is that type of surgery effective for a herniated disk?
ANSWER: Minimally invasive surgery can be an effective way to treat a herniated disk that has not responded to conservative, nonoperative treatment. Before you move forward, you should go through a comprehensive assessment to ensure that you are a good candidate for the procedure. If you are, this type of surgery often results in shorter recovery time and lower risk of complications than traditional spine surgery.
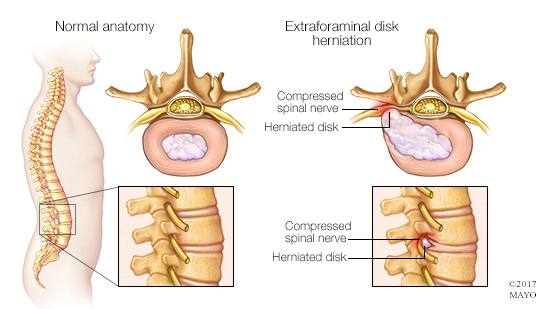
Spinal intervertebral disks are joints located between the spine bones, called vertebrae. The vertebrae and the disks stack up to create your spine. The disks serve as cushions between the vertebrae. They have a soft center wrapped within tougher exterior layers. A herniated disk happens when some of the softer material pushes out through a crack in the outer layers of the disk. A herniated disk may irritate or compress a nearby spinal nerve root. The result can be back pain or neck pain, along with pain, numbness or weakness in an arm or leg.
As in your case, treatment for a herniated disk begins with nonoperative therapy, such as medication and physical therapy. Injections also can be considered. If those do not work, or if you have severe pain or weakness, then surgery may be recommended.
The traditional procedure used to treat a herniated disk surgically is called a diskectomy. During this surgery, a surgeon makes an incision in the back, moves aside the muscles and tendons around the spine, and removes the part of the disk that is placing pressure on the nerve. In some cases of multiple, recurrent disk herniation, the entire disk may need to be removed. That’s uncommon, but, when it happens, the surgeon usually fills the space with a piece of bone. And the vertebrae on either side are fused together with metal hardware.
With minimally invasive spine surgery, the surgeon makes a smaller incision in the skin, usually about 16 to 18 millimeters long. Then small tools are inserted through the skin and muscle to access the disk and remove the damaged portion.
One of the benefits of minimally invasive surgery is that it does not require the surgeon to move aside the muscles or tendons near the spine. Leaving them in place decreases the amount of recovery time needed after surgery. It also may lower the risk of problems following surgery, such as adjacent segment disease — a condition in which degeneration develops in the sections of the spine above and below the treated disk.
Minimally invasive spine surgery is not right for everyone. When spine problems involve multiple herniated disk segments or additional spine disease, this approach may not be appropriate. A thorough evaluation prior to surgery that includes X-rays, an MRI and, less commonly, a CT scan can identify if your situation would benefit from a minimally invasive approach to herniated disk surgery.
Talk with your surgeon about the specific benefits and risks associated with minimally invasive spine surgery in your case to help you decide if this type of surgery might be right for you. — Dr. Mohamad Bydon, Neurosurgery, Mayo Clinic, Rochester, Minnesota







