-
Science Saturday: Will a machine pick your next medication?
What once may have seemed like a scene from a 22nd century sci-fi movie is reality today. High-speed, big data processing computers combine artificial intelligence with human know-how to crack complex health care conditions. This deep computer analysis may unveil new patterns that could bolster your health care provider’s ability to prescribe precise therapies, make a diagnosis, recommend a clinical trial or even predict your risk of disease.
Mayo Clinic Center for Individualized Medicine (CIM) is collaborating with the Coordinated Science Laboratory (CSL) at the University of Illinois at Urbana-Champaign (Illinois) to unleash the potential of artificial intelligence in patient care. Funded by a National Science Foundation (NSF) grant, the Mayo Clinic and University of Illinois Alliance and corporate partners are conducting research into the big data challenge: how to develop computer systems that, combined with human intelligence, unlock new analysis of health and disease.
Identifying depression therapy
Research within CIM is probing whether artificial intelligence can reduce or eliminate the trial and error of prescribing antidepressant medication. In a clinical study with Mayo’s Department of Psychiatry, researchers have combined machine learning ─ a type of artificial intelligence ─with genomics, metabolomics and other clinical variables. This machine learning approach helps health care providers to choose a therapy most likely to work on the first try.
“We combined expertise from clinicians, engineers and biologists to create an algorithm that uncovered patterns of antidepressant response that each of these specialists alone might not be able to recognize,” says Arjun Athreya, a Mayo Clinic and Illinois Alliance predoctoral research fellow. “Using this data with deep machine learning, we were able to predict with 75-85 percent accuracy whether a common antidepressant drug would work for each individual patient in the study. That compares to 58 percent accuracy when predictions are based only on clinical, demographic and social factors. In addition, we found that women and men respond differently to this antidepressant therapy.”

“This example shows the power of machine-based learning and methodology,” says Liewei Wang, M.D., Ph.D, co-principal investigator on the NSF grant. “This innovative approach uses psychiatric assessments, biological and molecular data and genetic traits in a predictive model. That is different than trying to uncover patterns using traditional sociodemographic variables, which are known to be weaker predictors. It tells us that a machine learning, artificial intelligence approach holds promise for identifying personalized therapies to address unmet patient needs.”
The research brings together massive amounts of genomic data and patient health that providers may also use to predict:
- Whether a patient is at risk for developing disease
- Whether a gene might influence how a drug works
“Using these machine learning approaches, instead of saying a drug is going to be effective 50 percent of the time for the average population, we can say, ‘Based on this person’s genetic and molecular makeup, here is what is going to be most effective for that individual,'” says Illinois' Ravishankar Iyer, Ph.D., co-principal investigator for the NSF grant. “These are methods that are pushing the boundaries of engineering and at the same time pushing the boundaries of medicine.”
How it works
Artificial intelligence is also called augmented human intelligence. It scans data and uses statistical methods, probability systems, graphical models, machine learning and deep learning to find patterns and make statements, decisions or predictions that may be difficult for the human mind to arrive at. One thing it won’t do, Dr. Iyer says, is replace the human health care provider.
“We’re not saying the machine is going to outwit the clinician or the surgeon. We are saying there is a knowledge the physician brings, and we use the high-level computing to augment that knowledge to personalize the prediction for an individual,” says Dr. Iyer.
Faster diagnosis and treatment
Mayo Clinic is studying ways artificial intelligence could improve many areas of patient care. One example is in radiology. Machine learning has the potential to improve the diagnostic accuracy of radiologists by automatically processing thousands of images generated during an imaging exam to identify the most important or key images. In doing so, time and effort are saved by identifying the most relevant images that can identify the cause of a patient’s symptoms. Another example is applying machine learning to the electronic medical record. An artificial intelligence analysis could help providers uncover patterns that identify disease subtypes, predict resistance to certain treatments or give a prognosis.
Some other artificial intelligence applications in research include:
- Predicting effectiveness of drugs for Alzheimer’s disease
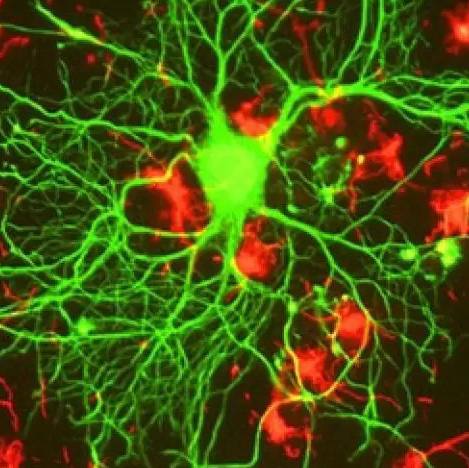
- Understanding how memory systems work in the brain and predicting how people learn
- Identifying breast cancer therapies shaped to each patient’s individual genetic code
- Using imaging to identify the genetic makeup of brain tumors without surgery
National Science Foundation Grant
CIM and the University of Illinois (Institute of Genomic Biology and the Coordinated Science Laboratory) are leading the National Science Foundation grant efforts to advance machine learning through work of the Center for Computational Biotechnology and Genomic Medicine (CCBGM). The five-year research grant mobilizes leaders in health care, academia and business to build sophisticated technology capable of interpreting massive genomic data at the point of patient care.
“Our goal is to produce as many high-performance computational models as possible —computer software or hardware — that will advance artificial intelligence and machine learning and bring that to market,” says Dr. Wang.
Dr. Wang says progress is being made, and she can foresee a day when artificial intelligence will be more widely applied in clinical care.
“I cannot say exactly when this will happen, but it will probably happen sooner than we’d imagine,” says Dr. Wang.
###
Additional research related to this article can be found online.
Join the conversation
For more information on the Mayo Clinic Center for Individualized Medicine, visit our blog, Facebook, LinkedIn or Twitter at @MayoClinicCIM.
See highlights from our recent Individualizing Medicine Conference 2017: Advancing Care Through Genomics:
- #CIMCon17 is underway
- #CIMCon17 continues with the microbiome and more
- #CIMCon17 day two explores how precision medicine can improve population health
- #CIMCon17 - precision-medicine for smoking cessation, rare diseases and cancer screening
Save the date for next year’s Individualizing Medicine Conference. It will be held Sept. 12-13, 2018.
###