 DEAR MAYO CLINIC: Who’s most at risk for developing sepsis, and what are the symptoms to watch for? What’s the difference between sepsis and septic shock?
DEAR MAYO CLINIC: Who’s most at risk for developing sepsis, and what are the symptoms to watch for? What’s the difference between sepsis and septic shock?
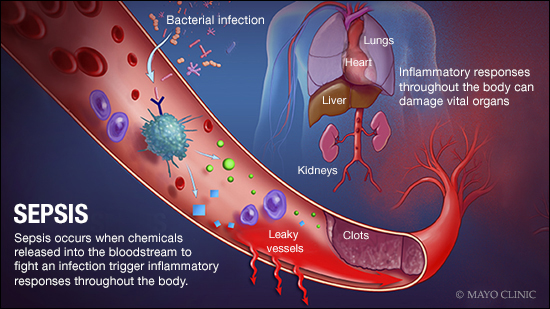
ANSWER: Sepsis is a serious complication of an infection. It often triggers various symptoms, including high fever, elevated heart rate and fast breathing. If sepsis goes unchecked, it can progress to septic shock — a severe condition that occurs when the body’s blood pressure falls and organs shut down. Sepsis most often affects the elderly, infants and people with weak immune systems, as well as those who require medical devices.
When you get an infection, your body releases chemicals into your bloodstream to fight off the infection. In some cases, those chemicals can trigger inflammation throughout the body. That inflammatory response is sepsis. If it’s not treated promptly, sepsis can progress, lowering blood pressure and making it hard for blood to reach vital organs. As a result, the heart, lungs, brain and kidneys all can be damaged. If it continues, sepsis can develop into septic shock, a life-threatening situation in which organs begin to fail and blood pressure drops even more dramatically.
Any kind of infection can trigger sepsis. But certain infections, such as pneumonia, abdominal or kidney infection, and infections that affect the blood, are more likely to cause sepsis.
Age is a significant risk factor for sepsis. The elderly and the very young are at higher risk because the immune system tends to be weaker in elderly adults, and it’s not fully developed in infants.
Other people with weak immune systems are more vulnerable to sepsis, too. Many people have weakened immune systems due to medical conditions, such as diabetes or HIV/AIDS. Some medical treatments, including medications taken after an organ transplant and after certain cancer treatments, can weaken the immune system. A severe illness that requires hospitalization also can lead to problems with a person’s immune system, raising the sepsis risk.
Individuals who need a medical device, such as a pacemaker, prosthetic joint, IV catheter or a breathing tube, are at higher risk of developing sepsis, as are those who’ve had previous wounds or burns.
Sepsis develops quickly, and it can be difficult to identify in its early stages. Symptoms include high fever, fast heart rate and rapid breathing. As sepsis worsens, it can trigger an abrupt change in mental status, such as disorientation or confusion. A significant decrease in urine production usually is a sign that sepsis is affecting the kidneys and other vital organs.
If someone who has an infection begins to experience sepsis symptoms, it is critical that he or she gets medical care right away. Hospital staff members watch patients closely for sepsis, particularly those in the emergency department and in ICUs. Patients diagnosed with sepsis receive plenty of IV fluids and are immediately given antibiotics.
People who have sepsis may require hospitalization. In addition to antibiotics, other medications may be used to treat symptoms such as low blood pressure. People whose conditions progress to septic shock often require care in an ICU, where they receive oxygen and IV fluids. They also may need a machine to help them breathe.
The longer sepsis is allowed to progress, the higher the chances it will become life-threatening. Research has shown, however, that if treatment is started within the first few hours from the time sepsis begins, the mortality rate from sepsis falls significantly. That makes early, aggressive treatment of sepsis crucial. If it is caught quickly, sepsis often can be managed effectively. — Dr. Alice Gallo De Moraes, Pulmonary and Critical Care Medicine, Mayo Clinic, Rochester, Minnesota
****************************
Related Articles
- Mayo Clinic Q and A: Understanding and preventing gangrene published 12/5/17
- Mayo Clinic researchers find protein that weakens severe sepsis immune reaction published 1/10/17







