-
Cancer
Women’s Wellness: Vaginal atrophy after breast cancer

Breast cancer and its treatments can cause many changes in your body. In addition to breast-related changes, you might also experience menstrual changes, hair loss or skin changes. In some cases, these changes can cause sexual challenges.
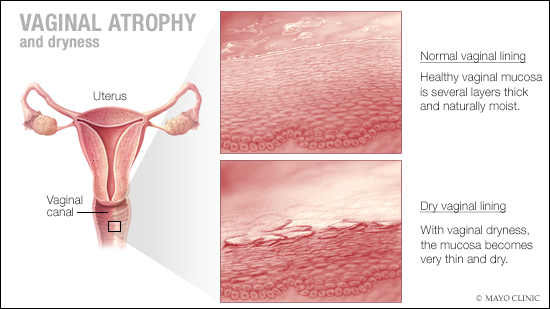
Vaginal atrophy, a thinning, drying and sometimes irritation of the lining of the vaginal walls, can be one of these challenges.
Vaginal atrophy is common as women age, but it can be worsened in women who've had breast cancer and are receiving endocrine treatments like tamoxifen or aromatase inhibitors.
Other situations that can result in vaginal atrophy include surgically induced menopause, and certain radiation therapies and chemotherapies.
Vaginal atrophy can make intercourse painful due to vaginal dryness or irritation and decreased lubrication. It can also lead to urinary symptoms like burning with urination, urinary urgency, incontinence and urinary tract infections.
Finding relief for vaginal dryness
When you've had breast cancer, non-hormonal options are the first choice for managing vaginal atrophy. This is particularly true if you've had a hormone dependent (estrogen and progesterone receptor positive) cancer. These options include:
- Vaginal moisturizers. Over-the-counter products like K-Y Liquibeads, Replens and Sliquid Satin can be used to restore moisture to the vaginal walls. These are typically applied several times a week, usually at bedtime.
- Lubricants. These nonprescription products improve discomfort from intercourse by reducing friction.Organic water-based or silicone-based hypoallergenic lubricants — like Yes, Jo and Sliquid — are less likely to cause vaginal irritation than are products that contain oil. Avoid products containing Vaseline.
- Allowing time for arousal. The natural lubrication created from sexual arousal can help reduce symptoms.
- Vaginal DHEA (prasterone). Talk to your cancer specialist about weighing the pros and cons of the different types of estrogen therapy.
Systemic hormone therapy generally isn't recommended. And cancers that are hormonally sensitive may also limit the use of vaginal estrogen options. This is especially true for women using aromatase inhibitor therapy to reduce the risk of cancer recurrence.
If your symptoms are bothersome even after trying the above steps, ask your health care provider about other options that may help. He or she can help you weigh your individual risks and decide on a specific plan.
If you have a history of breast cancer, tell your health care provider and consider these options:
- Nonhormonal treatments. Try moisturizers and lubricants as a first choice.
- Vaginal dilators. Vaginal dilators are a nonhormonal option that can stimulate and stretch the vaginal muscles. This helps to reverse narrowing of the vagina.
- Vaginal estrogen. In consultation with your cancer specialist (oncologist), your doctor might recommend low-dose vaginal estrogen if nonhormonal treatments don't help your symptoms. However, there's some concern that vaginal estrogen might increase your risk of the cancer coming back, especially if your breast cancer was hormonally sensitive.
- Systemic estrogen therapy. Systemic estrogen treatment generally isn't recommended, especially if your breast cancer was hormonally sensitive.
This article is written by Mayo Clinic Staff. Find more health and medical information on mayoclinic.org.








