-
Science Saturday: The science behind the test for the COVID-19 virus
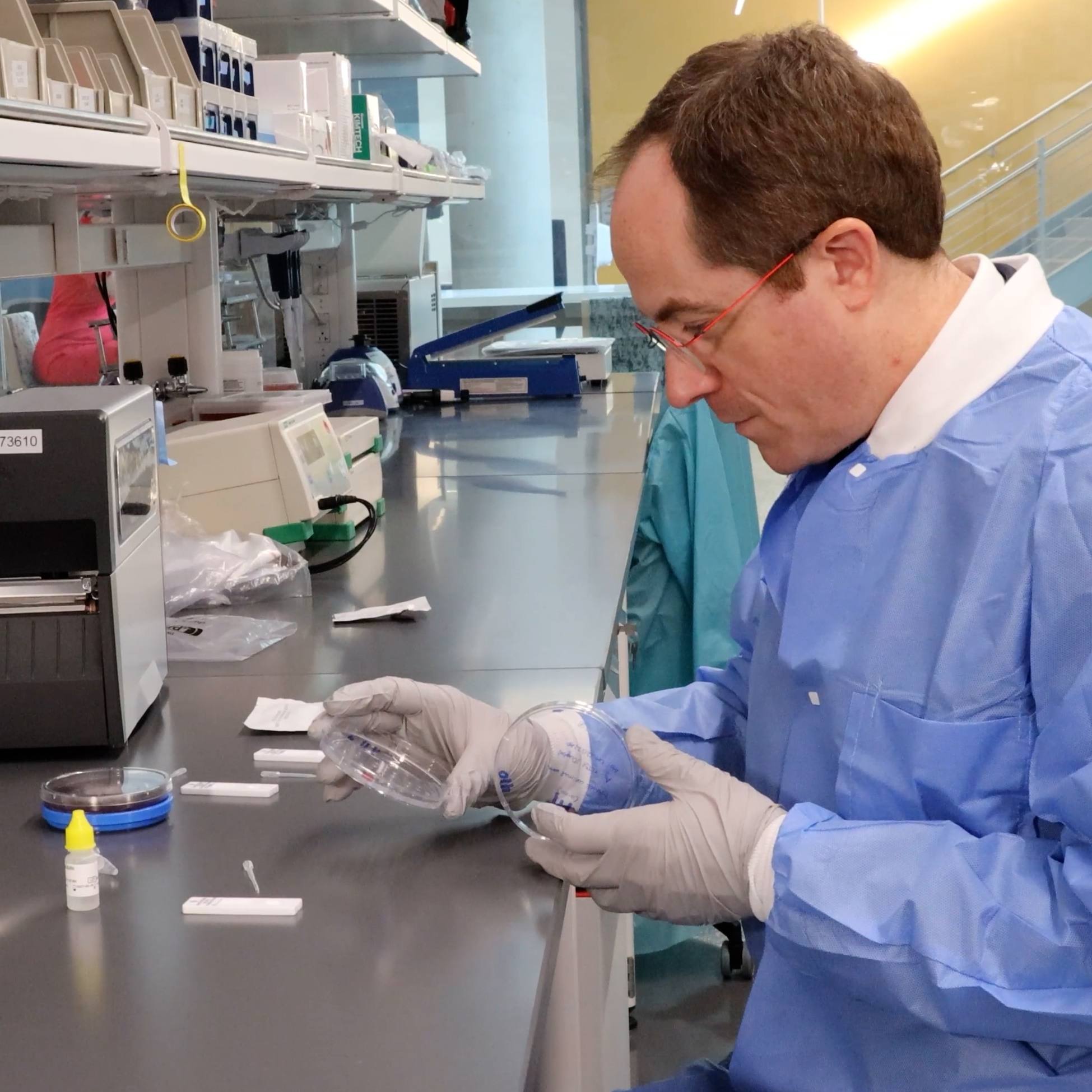
Mayo Clinic's new test for the virus that causes COVID-19 is described in a recent news release as a PCR test. While most won't know what that means, PCR is a well-used tool in the laboratory and medical testing. Larry Pease, Ph.D., a Mayo Clinic immunologist and the Gordon H. and Violet Bartels Professor of Cellular Biology; and Kyle Rodino, Ph.D., a clinical microbiologist, explain how this test works.
To start, PCR stands for a laboratory technique known as polymerase chain reaction. In this test, the goal is to selectively amplify trace amounts of genetic material, identifying specific parts of DNA. Just as a reminder, DNA is the genetic code that is present in every cell in the body. When a cell divides, it copies DNA, separating the two strands and then creating a new strand of DNA by copying the template. PCR mimics what normally happens in cells.

But why DNA?
DNA is used because at the most discriminating level, the structure of DNA can tell you what organism is being looked at. In the case of humans, PCR can identify a person using his or her genetic signature. In the case of COVID-19, researchers have published more than 100 genomes collected from patients to identify key features of the virus that causes that disease, SARS-CoV-2.
But there's a wrinkle.
PCR only works on DNA, and the COVID-19 virus uses RNA as its genetic code. RNA is similar to DNA, but only has a single strand. Fortunately, viral enzymes to convert RNA into DNA were discovered decades ago, and have been harnessed, along with PCR, to find unique signatures in RNA, too. In this case, PCR is referred to as reverse transcription PCR, or RT-PCR.
This is how it works.
First a person with symptoms of COVID-19 calls his or her local health care provider and asks how to be evaluated. Remember: Call first. Don't go to your clinic or hospital without calling to find out the safest way to get tested. Once a patient arrives at a safe testing site, a sample is taken by the health care team. Usually that means a narrow swab is placed in a person's nose or mouth to collect cells from the back of the throat.
"An upper respiratory specimen, particularly a nasopharyngeal swab, is the most common sample collected to reliably detect the virus," says Dr. Rodino. "Some lower respiratory samples like sputum are also acceptable in some settings."
At the lab, the sample is processed so RNA is isolated and collected. Everything else is removed. The RNA is mixed with other ingredients: enzymes (DNA polymerase and reverse transcriptase), DNA building blocks, cofactors, probes and primers that recognize and bind to SARS-CoV-2.

Then the viral RNA is converted to a DNA copy, and that single copy is then converted into millions of copies using PCR that can be easily detected.

The process is as follows: Using heat and enzymes, converted viral DNA strands are forced apart. Short primers of DNA matching the complementary strand of the viral DNA template stick together, functioning as an artificial start site for DNA synthesis.

Chemical building blocks of DNA are added and joined together, extending the synthetic DNA primer to form a copy of the viral DNA template. A second primer made in the opposite orientation downstream of the first primer is also present in the reaction. This makes a copy that is complementary to the first synthesized strand.
After one round of DNA synthesis, the reaction mixture is heated to melt the two strands apart, generating two templates that can be amplified further in the next round. The copies accumulate, round by round, exponentially, so that millions and millions of copies are generated to be studied using conventional approaches.

Because the enzymes and chemicals added to the reaction tube are relatively heat-resistant — "The heat sensitive enzymes are isolated from thermal resistant bacteria from hot springs," says Dr. Pease — the reaction can proceed in an automated fashion of heating, cooling and DNA synthesis. It only takes hours to complete the assay and get the results.
If SARS-CoV-2 complementary DNA is present in the sample, the primers can copy the targeted regions. As they copy these regions, probes stuck to these new fragments release a visual signal that can be read by the instrument used in this process.
"The millions of copies amplify this signal so it can be easily detected as a positive result. If the virus is not present, the probes do not stick, there is no signal release and it is a negative result," explains Dr. Rodino.
This type of analysis is used for research and clinical lab testing. PCR can detect all types of bacteria, parasites, viruses and fungi, starting with DNA or RNA. While the principle and ingredients are similar, each use requires specific primers or probes to detect different organisms. That's why something for SARS-CoV-2 had to be developed from scratch. During development, these sorts of tests are tweaked to make sure they are very good at detecting the organism of interest (sensitive) and making sure the test does not show a positive result when the organism is not there (specific).
"The importance of the steps involved in PCR has been recognized by a series of Nobel prizes over decades," says Dr. Pease. "Medical science advances as a result of basic discoveries about the molecular basis of living systems, and this is one example of how these discoveries come together to solve an important problem in our lives."
Working as a research and clinical team, Mayo experts were able to roll out a PCR test for SARS-CoV-2 in a matter of weeks ― shaving down what typically takes months to years.
"As the COVID-19 outbreak increased in size and scope, our leadership team made the decision to forge ahead with developing a novel PCR test to diagnose patients with this infection," says Matthew Binnicker, Ph.D., a clinical microbiologist and director of the Clinical Virology Laboratory at Mayo Clinic. "We made this decision because we knew that our providers at Mayo Clinic, as well as providers around the country, would need a laboratory diagnosis to make important patient management decisions. It was only through the collective efforts of a team of devoted laboratory professionals that we were able to deliver a test for COVID-19 in just three weeks. This was an extraordinary accomplishment that was fueled by Mayo Clinic's mission to provide hope and healing to the patients we serve."
― Sara Tiner, March 27, 2020