DEAR MAYO CLINIC: A woman I work with was diagnosed with ovarian cancer two years ago at 60. She reportedly was having a lot of abdominal bloating and pain on one side after meals. I heard she had a recurrence recently, and I am starting to worry since I have recently begun experiencing bloating after eating. I also have had some pain during menstrual cycles. I'm only 42. Is it possible I could have ovarian cancer? Is there a screening test? What are the treatment options?
ANSWER: Ovarian cancer is estimated to affect more than 22,000 women each year, and it is the fifth leading cause of cancer deaths among women, according to the American Cancer Society. While most of these women are over 60, ovarian cancer can affect younger women.
Unlike other gynecologic cancers, there are no screening tests for ovarian cancer. While some women diagnosed with ovarian cancer have elevated levels of the CA 125 protein, the associated blood test is not accurate enough for ovarian cancer screening, as many noncancerous conditions can increase the CA 125 level.
Ovarian cancer is hard to detect in its early stages due to its vague symptoms, which may often be mistaken for more common benign condition. Women may experience constipation, bloating, early satiety after eating and back pain. Discomfort in the pelvic area and change in bowel habits, including a frequent need to urinate, also may be symptoms of ovarian cancer.
While some discomfort during menstruation may be expected, any pelvic pain, coupled with the other symptoms you mentioned, would be reason to reach out to your primary health care provider or make an appointment with a gynecologist. Your health care provider also can guide you on your personal risk related to ovarian cancer.
Endometriosis is a common condition that is associated with ovarian cancer. Other conditions that may affect a woman's risk include smoking, polycystic ovary disease and obesity.
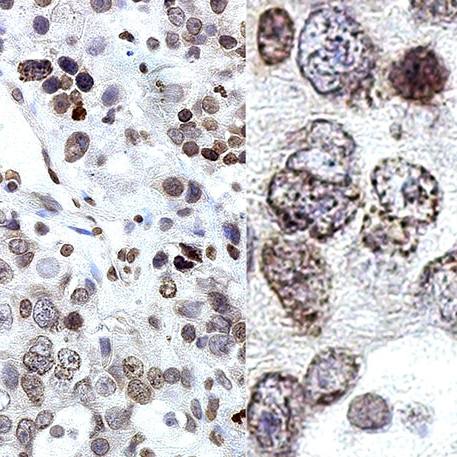
About 10% to 15% of all ovarian cancers are caused by a genetic mutation. The genes that are well-known to increase the risk of ovarian cancer are BRCA1 and BRCA2. These genes also affect a woman's risk of breast cancer. Genetic mutations that cause Lynch syndrome, an inherited condition associated with colon cancer and uterine cancer, also raise a woman's risk of ovarian cancer. In addition to these genes, there are many other less common genetic abnormalities that can be detected easily through blood or saliva testing.
For woman who have a family history of breast cancer, colon cancer or ovarian cancer, or have a family member who is positive for a genetic mutation, it may be valuable to speak to a genetic counselor to discuss genetic testing. If she has that genetic mutation, relatively easy surgery can be performed to significantly decrease the risk of developing ovarian cancer. For patients who are still interested in having children, taking birth control pills is an easy option to decrease the risk and still preserve fertility. Traditionally, there have been few options to treat ovarian cancer other than surgery and chemotherapy, and recurrence of the disease has been common. Now, thanks to advances in research, individualized medical therapy and immunotherapy are providing new treatment options for ovarian cancer patients.
There are more than 1,300 clinical trials for ovarian cancer, including a vaccine trial aimed at preventing recurrence. Some women also may be candidates for something known as hyperthermic intraperitoneal chemotherapy, which is performed in conjunction with cancer surgery. After a surgeon has removed all the visible cancer from inside the abdomen, high-dose chemotherapy is delivered directly to cancer cells inside the abdominal cavity. One of the significant benefits of hyperthermic intraperitoneal chemotherapyis that it allows for a high dose of chemotherapy to be given to the area that needs it, and it's been shown to improve survival. — Dr. Tri Dinh, Obstetrics and Gynecology, Mayo Clinic, Jacksonville, Florida
****************************
Related Articles
- New therapies bring hope for ovarian cancer published 9/25/19
- Living With Cancer: Ovarian cancer risk after hysterectomy published 1/11/19
- Women’s Wellness: Some answers about ovarian cancer published 1/3/19