It's not every day that a virtual hospital moves into a family home. But that's what happened after John Rohrscheib contracted COVID-19.
On Nov. 4, the 84-year-old retired implement dealer had serious leg pain and a fever. He and Joanne figured the pain was due to an accident from the previous year, but they wanted to get it checked out. So they traveled to the Emergency Department at Mayo Clinic Health System in Eau Claire, Wisconsin.
During that visit, John was tested for COVID-19 because he had a fever. He was sent home that evening, but he received a call the next day to let him know that his COVID-19 test was positive.
"We were shocked," says Joanne, 83. "I figured if he had it, then I had it, too, since I drive him to his appointments."
John needed to return to the Emergency Department on Nov. 7 because he was having trouble breathing at home and the pain in his legs had worsened. This time, he was admitted to the hospital.
"When I went in, I was short of wind," John says. "They did a good job for me and got me started on meds right away."
While in the hospital, he received his first dose of remdesivir — an antiviral drug that prevents the COVID-19 virus from copying itself.
"Most hospitalized patients who are positive for COVID-19 and have symptoms of the virus, such as shortness of breath, require a daily dose of remdesivir for five days. It is given intravenously, so this occurs while the patient is in the hospital," says Margaret Paulson, D.O., a Mayo Clinic Health System hospitalist. "However, there is a new option for patients with conditions previously managed in a hospital called advanced care at home."
Dr. Paulson also is the chief clinical officer for advanced care at home. The program delivers comprehensive, complex care to patients from the comfort of home through high-quality virtual and in-person care and recovery services. Patients in the program are monitored virtually 24/7 by a physician-led care team from a command center using technology installed in patients' homes to track vital signs, medications and infusions.
The team virtually connects through video with patients at home, where paramedics, nurses or other support team members are available to oversee medications, IV fluids or otherwise be the care team's hands.
While John was in the hospital, Kasey Peissig, the nurse manager for the advanced care at home program, explained the service to the couple.
"John was a good candidate for the program because his medical condition was relatively stable but still required an acute level of care," Peissig says. "We would be able to meet all his care needs in the comfort of his home through this program."
After discussing the program, John and Joanne decided it was the right option for them.
"John has had home health care before, but I knew this was different," Joanne says. "We knew we wanted to try it and see. And I knew they were short of beds."
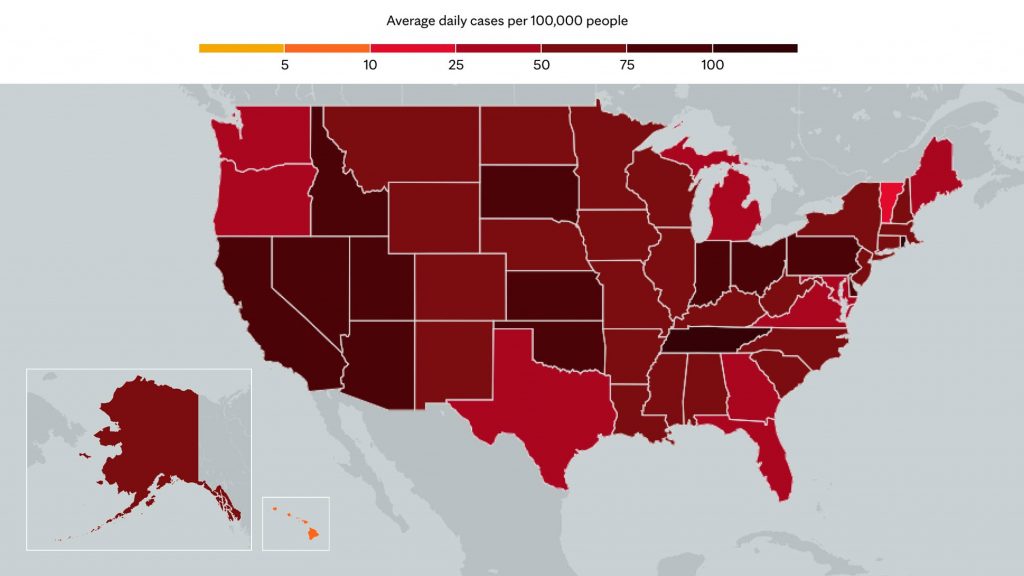
An increase in COVID-19 cases in the area had led to a rise in the number of patients requiring hospitalized care and full hospitals across the region.
"Unfortunately, there have been recent instances when 100% of our hospital beds were full. The advanced care at home program helps us safely decompress the hospital and open beds for other patients," Dr. Paulson says. "Every little bit helps during these challenging times, and advanced care at home is an example of how we are evolving to meet the health care needs of our communities."
After three days in the hospital, John was transferred home and admitted into the advanced care at home program on Nov. 10.
A team of nurses, community paramedics, advanced-practice providers, doctors and other health care professionals brought the hospital to the couple's home, including the technology that would connect him to his virtual care team.
"Not every patient who is positive for COVID-19 will qualify for this service, but for those who do, it can be a game-changer," Dr. Paulson says. "It lets them recover safely at home and allows the care team to be at the patient's bedside 24/7 at the push of a button, which can be very reassuring for them when they are acutely ill."
Having advanced medical technology in their home didn't scare John or Joanne.
"They wheeled him in the house and started setting everything up. They made sure everything was working and showed me how to use it. It was very clear and very simple," Joanne says. "I didn't have to worry if he was having trouble breathing or was uncomfortable because I could just call for help. The team helped us feel very comfortable with all of it."
Their attitude doesn't surprise Peissig.
"Both he and Joanne were very interested in participating in our program and did well with the technology," she says. "They described themselves to me as interested in learning and enjoy having new experiences, so this was a good fit."
John received hospital care at home for two additional days. During that time, the team monitored his vital signs, assessed his overall health condition, drew blood for a lab test and gave him the last dose of remdesivir. He was discharged from the advanced care at home program on Nov. 12.
Another program benefit during the COVID-19 pandemic was that John and Joanne could remain together during his recovery. Visitor restrictions in the hospital would have prevented Joanne from being at John's bedside, especially as Joanne tested positive for COVID-19 a few days later. So far, her symptoms have been mild, and they have been able to recover together.
The couple is looking forward to getting back into a routine after the pandemic. For John, that includes daily 6 a.m. coffee time with his friends, and mowing his lawn at his home and at his son's farm. Joanne is looking forward to altering clothes, and spending time with her 10 grandchildren and six (soon-to-be seven) great-grandchildren.
The Rohrscheibs say they highly recommend the program and the care team to others.
"The nurses were always so pleasant," says Joanne. "They took their time and made sure you understood they were there to help. They made you feel like they were enjoying what they were doing."
__________________________________________
Information in this post was accurate at the time of its posting. Due to the fluid nature of the COVID-19 pandemic, scientific understanding, along with guidelines and recommendations, may have changed since the original publication date.
For more information and all your COVID-19 coverage, go to the Mayo Clinic News Network and mayoclinic.org.
Learn more about: Tracking and trending COVID-19
Related Articles