-
Racial Disparities in Myeloma Treatment Nationwide
Blood cancer specialist Sikander Ailawadhi, M.D., was working in a county hospital in California several years ago when he became aware of a trend in cancer care that was concerning.
“I noticed patient profiles from different racial subgroups seemed to get different treatments and have different outcomes,” says Dr. Ailawadhi, a specialist in multiple myeloma and now vice chair of clinical practice for hematology on Mayo Clinic’s campus in Florida.
Those observations led to an investigation of health disparities across the country among patients with myeloma published in the journal Cancer.
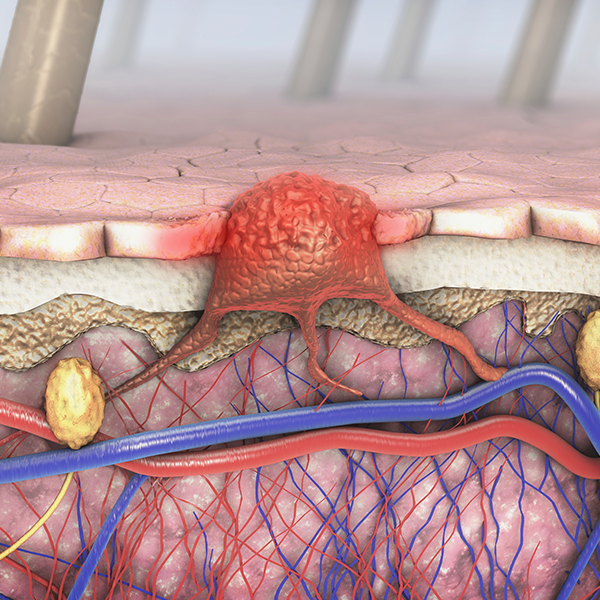
Multiple Myeloma
A complex cancer of the white blood cells, myeloma is rare. It affects about 100,000 people in the U.S. according to 2014 data and while incurable, it is treatable.

To examine care for myeloma patients, Dr. Ailawadhi's group looked at nearly 20 years of medical records from two sources, the Surveillance, Epidemiology, and End Results (SEER) database of the National Cancer Institute, and Medicare. These data allowed the team to scrutinize long-term trends and multiple factors involved in care.
“We were interested in looking at symptoms, how patients are managed, cost of care, and outcomes, and whether these have been changing over time, and whether there are differences for various racial subgroups,” he says.
The study explored data for nearly 36,000 patients nationwide, including the US Census groups: White, Black, Hispanic, Asian, and others. The authors found that myeloma survival improved considerably during the time period studied (1991-2010). The proportion of patients receiving treatments—which include the integration of chemotherapies, drugs to boost the immune system, steroids, and stem cell transplants—also has been on the rise. Interestingly, Dr. Ailawadhi says, severe symptoms associated with inferior overall survival of the disease decreased between 2006 and 2010.
“We think that may be because patients are being diagnosed sooner, and more effective drugs have become available. Patients are showing less severe symptoms at the time of diagnosis,” Dr. Ailawadhi says.
Uneven Care
Even though the use of recommended drug combinations has become more common, disparities exist in the care patients tend to receive, according to the study. Black patients and whites more often received the anti-myeloma drug bortezomib and stem cell transplant, while Asian and Hispanic patients more often received steroids and immune-modulating drugs including lenalidomide and thalidomide. Black patients were found to have the most myeloma-related clinical symptoms the most frequently; but this group tended not to receive immunomodulatory drugs as often as their counterparts from other racial ethnic groups.
“We don’t know if the drugs are being prescribed differently, or patients have less access to treatments because of costs, or because of the types of clinics they have access to,” Dr. Ailawadhi says, explaining that the study found a decrease in the rate of death for individuals with higher income. The study also found that median cost of care for Medicare patients in the first six months after diagnosis of multiple myeloma increased from $5,110 in 1991 to $27,800 in the time between 2006-2010. Median drug-claims in the first six months were highest among blacks, according to the authors.
Encouragingly, says Dr. Ailawadhi, the differences in survival rates for patients of various races are becoming less pronounced but there’s more work to do. “Even though overall survival has improved, if we mitigate these disparities in drug use or access, we might boost the survival of certain subgroups even further. This study has provided more information for that conversation.”

The study was funded by the Cancer Focused Research Team at Mayo Clinic’s hospital in Florida. In addition to Dr. Ailawadhi, Mayo Clinic researchers from the Arizona and Minnesota campuses collaborated on this work.
More information can be found in the full article.