-
Mayo Clinic Q & A
Mayo Clinic Q and A: Thoracic aortic aneurysms

DEAR MAYO CLINIC: My friend was diagnosed with a thoracic aortic aneurysm. What causes this type of aneurysm, and how fast does it grow? Also, how are thoracic aortic aneurysms treated?
ANSWER: A thoracic aortic aneurysm occurs when one or more areas along the wall of the aorta — the body's largest blood vessel — becomes weak or damaged. The aorta carries oxygen-filled blood from the heart to the body, including the brain. With time, the pressure of blood flowing through the weakened area can cause it to enlarge or bulge — typically without signs or symptoms.
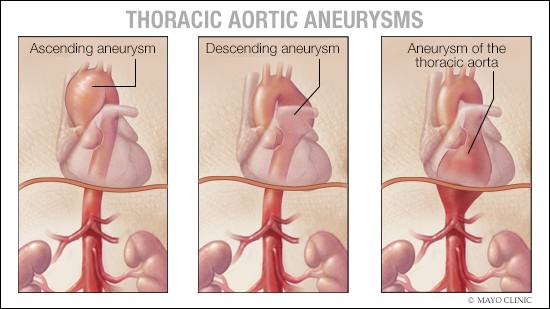
Most commonly, bulges occur in the abdomen, called an abdominal aortic aneurysm. However, aneurysms also can develop closer to the heart in the chest area, and these aneurysms can develop in the ascending aorta or descending thoracic aorta.
The main concern with aortic aneurysms in the chest is a tear, or dissection — or more seriously a rupture that allows blood to leak into the aorta's lining or into the body. With a dissection or rupture, it's important to quickly recognize these symptoms:
- Sharp, severe or sudden chest or upper back pain that radiates downward, or includes the jaw, neck or arms.
- Difficulty breathing or swallowing.
- Clamminess.
Immediate emergency care, including open-chest surgery, is necessary for a dissection or rupture. Unfortunately, dissections and ruptures often are fatal.
Most aortic aneurysms are small, and they develop slowly. They are discovered when imaging is performed on the chest or abdominal area for another reason.
A smaller aneurysm has a low risk of rupture — about 1% or less per year. For that reason, as long as it's not growing quickly, most health care providers will recommend a watch-and-wait approach. This means using imaging tests, such as echocardiogram or CT scans, at regular intervals to monitor the aneurysm's size and rate of growth. Health care professionals also may prescribe medications such as beta blockers. These are used to treat high blood pressure, which is present in about 60% of people with thoracic aortic aneurysms.
Typically, an aneurysm grows slowly, although it can grow faster, particularly in people with a family history of aortic aneurysms or with a genetic condition related to the body's connective tissues. If an aneurysm is larger or is found to be growing too quickly, elective surgery to repair the aneurysm may be considered. This may involve open-chest surgery or an endovascular option where a stent is placed to cover the aneurysm. The goal is to remove the damaged section of the aorta and replace it with a synthetic tube, or graft, or allow the blood to flow through the stent graft instead.
Men are much more likely than women to develop a thoracic aortic aneurysm. Most commonly, the condition starts to occur in people in their 50s and 60s, although it may not be detected until decades later, if at all.
A family history of aortic aneurysm puts you at increased risk. Genetic connective tissue disorders — Marfan syndrome, Ehlers-Danlos syndrome and Loeys-Dietz syndrome — dramatically increase your risk. Those born with just two, rather than three, leaflets, or cusps, of the aortic valve — a condition called bicuspid aortic valve — are at increased risk.
Other factors that increase the risk of a thoracic aortic aneurysm include high blood pressure; smoking; high cholesterol levels; and development of blood vessel hardening and clogging, or atherosclerosis.
People at highest risk — those with a family history plus one or more other risk factors — should ask their primary health care provider about having an echocardiogram to look for a thoracic aneurysm, even in the absence of signs or symptoms. Surgery generally is recommended for thoracic aortic aneurysms with a diameter of 5.5 centimeters or larger, and at smaller diameters, depending on the underlying cause of an aneurysm.
There are many professionals who can assist with this condition. A visit with a vascular or endovascular specialist or a cardiovascular surgeon may be warranted depending on the findings of the screening. — Dr. Young Erben, Vascular Surgery, Mayo Clinic, Jacksonville, Florida
****************************
Related Article







