Sarah Bradley's heart failed when she was only 27 years old. Today, after more than two years living with the assistance of a device that kept her blood flowing and her health stable, she’s the grateful recipient of a new heart.
Sarah Bradley's heart failed when she was only 27 years old. Today, after more than two years living with the assistance of a device that kept her blood flowing and her health stable, she’s the grateful recipient of a new heart.
For more than two years, Sarah Bradley lived with a broken heart. The muscle meant to move blood through her body failed when she was 33 weeks pregnant with her second son. And if not for the assistance of a medical device implanted and monitored by her care team at Mayo Clinic, she would not have survived the 26-month wait for a donor heart to become available to her for a transplant.
Sarah, who lives with her family in Roswell, New Mexico, was 27 and in her third trimester when she was diagnosed with a rare condition known as peripartum cardiomyopathy by her local physicians. Sarah was shocked to learn she was one of a small group of pregnant women with severe heart disease.
"The bad thing with heart failure is that is mimics a lot of things pregnant women go though: the swelling, not being able to breathe because your baby's up in your lungs," Sarah says. "The only thing I experienced that I knew wasn't right was my coughing. I would cough day and night, and nothing helped."
"I don't know if it's because I've always heard of Mayo as being the top hospital in the U.S., but getting there on the plane, I immediately felt at ease." — Sarah Bradley
Many women with heart failure can recover from it, but Sarah's physicians informed her that her heart was damaged beyond repair. Following the birth of her son in March 2015, she was airlifted from New Mexico to Mayo Clinic's Arizona campus.
"I don't know if it's because I've always heard of Mayo as being the top hospital in the U.S., but getting there on the plane, I immediately felt at ease," she says. "I knew that things were going to be taken care of, and I was going to be okay."
That sense stuck with Sarah during her long wait for a new heart, all the while living with the support of a mechanical device that kept her alive.
Receiving life-sustaining support
When she first arrived at Mayo Clinic, Sarah was rushed to the intensive care unit, where she met her cardiology care team. Physicians from the Division of Cardiovascular Diseases informed Sarah that her heart had likely been in failure for some time. As her heart worked harder to pump blood, it grew larger and became weaker.
"They started discussing that they needed to put me on the heart transplant list," Sarah says. "They also decided that the only thing that would keep me here was getting an LVAD implanted."
 An LVAD, or a left ventricular assist device, is a mechanical pump implanted into the heart that helps move blood from the heart's lower left chamber, or ventricle, to the rest of the body. Placed in Sarah's left ventricle in mid-March 2015, the device included a cord that exited Sarah's abdomen. That cord connected to a battery pack that Sarah either carried with her or, if she was sleeping or sitting at work, keep plugged into a wall outlet.
An LVAD, or a left ventricular assist device, is a mechanical pump implanted into the heart that helps move blood from the heart's lower left chamber, or ventricle, to the rest of the body. Placed in Sarah's left ventricle in mid-March 2015, the device included a cord that exited Sarah's abdomen. That cord connected to a battery pack that Sarah either carried with her or, if she was sleeping or sitting at work, keep plugged into a wall outlet.
"I called it my lifeline," she says. "It's like another piece of me that kept me alive."
Biding time
Devices like the one Sarah had often are considered bridge therapies to transplant. They are designed to last as long as 10 to 15 years. For example, Mayo Clinic is caring for one individual who's been supported by a ventricular assist device for more than nine years, says Jenifer Spadafore, a physician assistant in Cardiovascular Diseases.
"Even though I work with these patients, it's really hard to understand what they're going through as they're waiting for the phone to ring and that precious gift of life to be offered," says Spadafore, who was part of Sarah’s care team.
Because the time waiting for a transplant can be so stressful, Mayo Clinic works on resiliency training with those on the list for a new heart.
"We want to get them to live in that healthy lifestyle mindset that everyone needs: living in the moment, eating well," Spadafore says. "So we talk about that and encourage that."
"I came to realize that with the LVAD, I was still here and present, still able to watch my kids grow. I'd rather have that than get a heart that wasn't for me." — Sarah Bradley
Living with the device was not easy, but Sarah maintained a lifestyle that helped to keep her from dwelling on her situation.
"I tried not to think about it. My boys, being 5 and 2, kept me very busy," she says. "And it helped that I worked full-time, so I wasn’t just sitting and worrying about it. I came to realize that with the LVAD, I was still here and present, still able to watch my kids grow. I'd rather have that than get a heart that wasn't for me."
Sarah's attitude about her situation and her ability to manage her life despite its complexities amazes Spadafore.
"It's just a privilege and an honor to take care of her, because she gives so much back to us in the way that she lives her life and the way she takes care of her kids and family," Spadafore says. "She is very special."
Enjoying new freedom
Sarah’s patience was rewarded in April 2017 when she got the call, on Easter Sunday, that a heart was available.
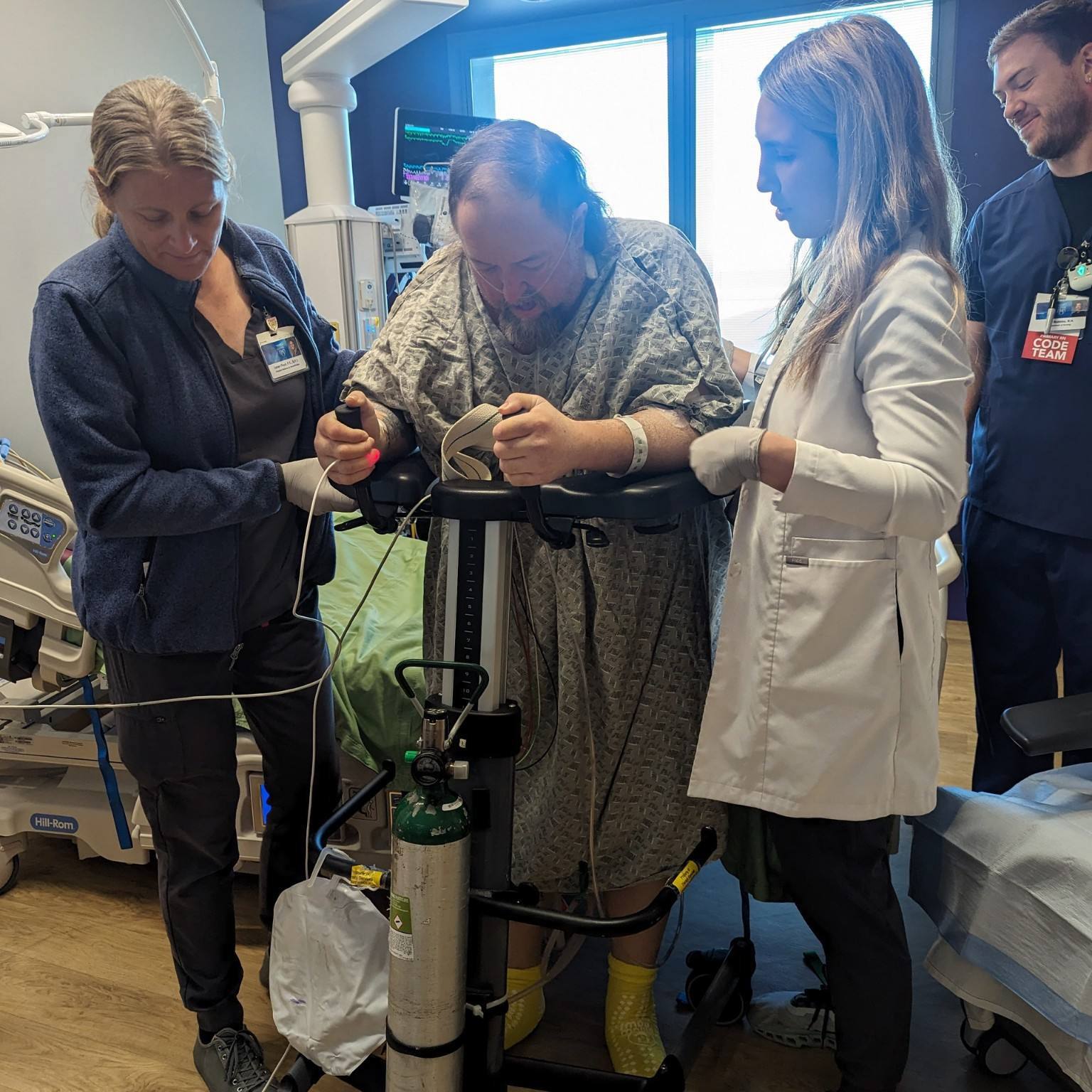
So far, Sarah says, her recovery after transplant is going as well as can be hoped for. Two biopsies to check for rejection have come back negative. And she is relieved that she no longer needs to be connected to a power source.
“My biggest fear right now is still going into rejection, but I feel amazing,” she says. “It’s definitely a change going from having a bag with me 24/7 to not having anything. I’m enjoying the freedom.”
Sarah will begin cardiac rehabilitation soon and is adjusting to the multitude of anti-rejection medications she will take for the rest of her life.
“But it’s so worth it,” she says.
From Sarah's perspective, her Mayo Clinic care team provided a major source of relief and comfort for her as they helped navigate her complex condition.
"Every time I get back to Mayo and see the hospital, I get this overwhelming sense of it being home," she says. "I just feel comforted going in, and I know that all of my doctors listen to all of my concerns. They care about how I'm feeling and what I'm going through."
HELPFUL LINKS
- Learn more about ventricular assist devices.
- Check out the Department of Cardiovascular Diseases.
- Connect with others talking about Heart Disease on Mayo Clinic Connect.
- Visit Mayo Clinic's Arizona campus.
- Request an appointment.
Related Articles