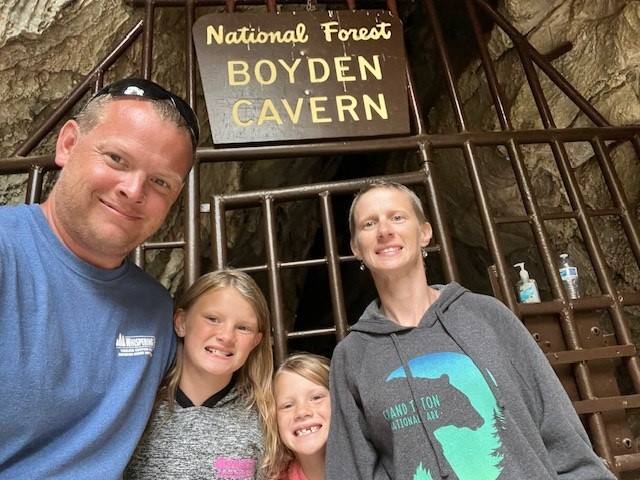
Stacy Weisensel and her husband Joshua had a goal: to take their daughters to as many national parks as possible. But in the summer of 2021, while trying to enjoy the breathtaking views of Yellowstone National Park with her family, Stacy was distracted by a nagging pain in her esophagus. Over the next few months, Stacy’s symptoms grew worse and ultimately led to a frightening diagnosis — stomach cancer.
A life-changing diagnosis
In July 2021, after returning from vacation to her home in Montello, Wisconsin, Stacy decided to see her primary care physician about the pain in her esophagus. Stacy’s doctor diagnosed her with acid reflux and prescribed an anti-acid medication, which seemed to help control her symptoms, at least temporarily.
“I went back to my doctor in November for my annual physical,” Stacy says. “I told her that I wasn’t sure the antacid medication was doing anything for me because I still had that pain in my esophagus, just not all the time.”
Stacy also had begun experiencing pelvic pain and her menstrual cycles were becoming irregular. Her doctor suggested she stop taking the antacid to see what would happen. If the pain worsened, they would consider a stronger medication.
At the end of November, with the pelvic pain growing unbearable, Stacy returned to her doctor, who ordered a pelvic ultrasound to be performed in early December.
But, on Dec. 7, just before that scheduled ultrasound, Stacy woke up with intense pain.
“I could barely get out of my car when I got to work at 5:30 that morning. I made myself go in, but I could only make it until 8 a.m.,” Stacy says. “I told my colleagues while bawling that I was in so much pain I had to go to the emergency room.”
Stacy drove 45 minutes to the closest hospital in Madison, Wisconsin, where she had an emergency pelvic ultrasound. But the results showed that nothing was amiss.
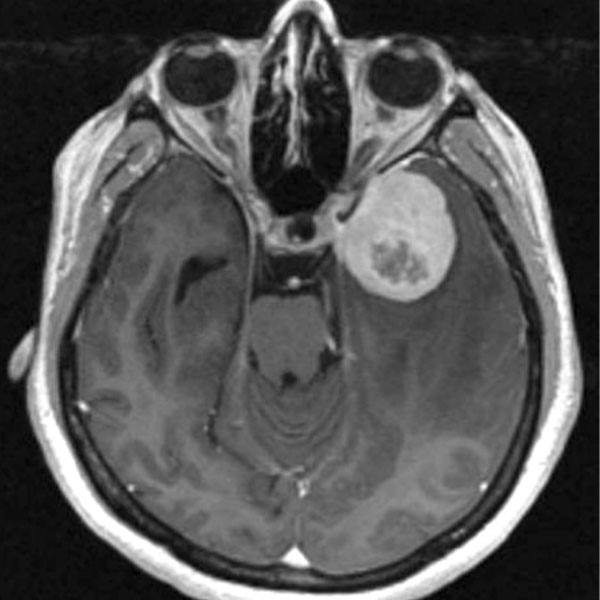
Thankfully, the care team proceeded to do a CT scan, which gave insight into Stacy’s intense pain. Stacy had an ulcer, an open sore that developed on the lining of her stomach. She underwent an endoscopy the same day so the team could collect tissues to biopsy.
Two days later, Stacy received a life-changing call — the biopsy came back showing cancer.
She was immediately referred to a local oncologist who completed a full staging workup. The results showed that the cancer had metastasized to Stacy’s ovaries. At 37 years old, Stacy’s official diagnosis was stage 4 stomach cancer.
“It was a lot for me when I got that phone call,” recalls Stacy. “My husband and I were devastated. But now we have to get a game plan together.”
Stacy immediately started a chemotherapy regimen, but her medical oncologist recognized she could benefit from receiving care at a center experienced with her type and stage of cancer. He referred her to Travis Grotz, M.D., a surgical oncologist at Mayo Clinic in Rochester, Minnesota.
Treating the visible and invisible
In February 2022, Stacy and Joshua traveled to Rochester to meet Dr. Grotz. He agreed Stacy should finish her chemotherapy but suggested she consider surgery and hyperthermic intraperitoneal chemotherapy, or HIPEC, something Stacy didn’t know was an option.
“We are seeing a worrisome trend as stomach cancer is being increasingly diagnosed in younger patients,” Dr. Grotz says. “The cause of this is unknown, but unfortunately younger patients like Stacy are diagnosed with more advanced cancers. We aggressively treated her cancer with both systemic and intraperitoneal chemotherapy.”
Combining surgery with HIPEC removes what the surgeon can and cannot see.
“Imagine cleaning a countertop,” says Dr. Grotz. “The surgery cleans up the dirt I can see, while the chemotherapy cleans the microscopic dirt I can’t see.”
HIPEC is performed after all visible cancer inside the abdomen is removed. Then, the abdominal cavity, or peritoneum, is bathed with a high dose of hot chemotherapy to kill any microscopic cancer cells that remain. Heating the chemotherapy drug allows it to penetrate the tissue more deeply, increasing the number of cancer cells it can reach.
Dr. Grotz says that performing HIPEC to treat stomach cancer is important because half of stomach cancer recurrences occur in the peritoneum. Doing surgery and HIPEC together increases the success rate and the likelihood that cancer will not return.
On May 12, 2022, Stacy underwent a 12-hour surgery that included removal of 80% of her stomach, lymph nodes, and a complete hysterectomy. After all the visibly cancerous tissue was removed, Dr. Grotz administered HIPEC, heated to about 108 degrees Fahrenheit, to target any cancerous cells left behind.
Because her operation was performed using minimally invasive, robotic techniques, Stacy recalls that within six hours of being transferred to her room, she could walk down the hallway with a walker. Three days later, she was discharged from the hospital. And after a follow-up appointment on May 19, Stacy returned home to her family in Wisconsin.
“Unlike many other centers, at Mayo Clinic, we use minimally invasive techniques to perform this operation and the HIPEC procedure,” says Dr. Grotz. “By utilizing robotic surgery, we can curb the length of hospital stay and reduce the rate of complications.”
Dr. Grotz continues that, with minimally invasive techniques, he can hopefully achieve good cancer outcomes while improving quality of life after surgery.


More summer trips on the horizon
As Stacy approaches the year mark after surgery, she and her family are busy planning their next big adventure.
“We obviously want to visit more national parks,” Stacy says. “We haven’t been to the Rocky Mountains yet, so maybe we’ll visit when we go to Glacier National Park.”
And on this trip, Stacy looks forward to fully enjoying the scenery thanks to the care she received at Mayo Clinic.
“At this point, I am cancer-free,” Stacy says. “I had the best care at Mayo Clinic, and am very grateful for what everyone did for me.”