-
The future will be personalized: Accelerating microbiome research
We’re in the midst of a microbiome research epidemic, according to Purna Kashyap, M.B.B.S., co-associate director of the Microbiome Program in the Mayo Clinic Center for Individualized Medicine. “We started early and are pushing hard,” says Dr. Kashyap. “We’re one of the top accelerators in the field and are well poised to move microbiome research findings to the clinic. We anticipate that happening in another decade or so.” Dr. Kashyap is a professor in the Mayo Clinic College of Medicine and Science.

Microbiome-related research at Mayo Clinic focuses on improving patient outcomes or bringing microbiome discoveries to clinical practice — an area in which Mayo Clinic leads. The Microbiome Program provides resources for Mayo Clinic researchers doing this work, providing knowledge and infrastructure assistance.
“Microbiome research is young, vibrant and ongoing,” says Dr. Kashyap. “We don’t have all the answers yet, but we know the microbiome is a component of multiple chronic diseases and an important contributor if not always the inciting factor.”
Dr. Kashyap’s Microbiome Program co-associate director, Nicholas Chia, Ph.D., concurs: “There is mounting evidence that changes in the microbiome may be implicated in the development, progression and treatment of multiple diseases. Eliminating dangerous microorganisms or restoring normal microbiota may reverse this process. This is a critical possibility that we are still learning more about.” Dr. Chia is an assistant professor in the Mayo Clinic College of Medicine and Science.
Microbiome research at Mayo Clinic includes studying the role of bacteria, fungi and viruses in disease states ranging from cancer to obesity and everything in between. A large trial of cancer patients is analyzing whether the microbiome can be used as a biomarker to predict cancer treatment response and adverse events. In another project, Mayo Clinic has licensed a bacteria to a biotechnology company for further study about its role in suppressing multiple sclerosis and rheumatoid arthritis. Another project Mayo collaborated on resulted in a commercial product to provide microbiome-directed personalized nutrition to regulate blood glucose and prevent complications of diabetes and prediabetes.
Dr. Kashyap compares microbiome research to genome research. “The human genome was sequenced in 1991. In 2022, we use it to predict risk and tailor disease treatment. That was one genome. Microbiome complexity is much higher, and we’re trying to do the same thing in terms of sequencing and understanding. We’re making progress and, while we stumble along the way, we have learned from early failures that which has positioned us well for future success. One way in which the microbiome is particularly exciting is that it is modifiable whereas genes are not.”
He predicts that the first FDA-approved microbiome-related therapies will be stool substitutes to reset the microbiome of the colon in patients who have Clostridioides difficile (C. diff) infection.
“In the future, we’ll be able to look at a person’s microbiome and tell a patient their risk of developing a disease, much like we do now with commercially available human gene panels. This holds promise as a preventive strategy because, unlike our genes, the microbiome can be changed. What we already see across the horizon in diseases such as cancer and autoimmune conditions is the ability of an individual’s microbiome to predict which treatments will be effective or have the fewest side effects and how a person might respond to different treatments so we can eliminate trial and error and start with the best treatment first. We also could try to change the microbiome with diet or prebiotics to improve chances of success with a treatment. But we’re not there yet. We’re moving at a fast rate, and I’m optimistic that we will have early wins by the end of this decade.”
In the meantime, Dr. Kashyap advises people interested in keeping their microbiome healthy to eat a high-fiber diet from diverse food sources. “Most chronic diseases have microbiomes that show low diversity. We know that a highly diverse state is more resilient to change, and a high fiber diet will increase the diversity of your microbiome.”
Moving the needle in GI motility
Dr. Kashyap’s own research focuses on the role of the microbiome in disorders of the gut–brain interaction and how bacteria affect the functions of the intestine, such as motility, which can be altered in these conditions. His lab found that bacteria can convert tryptophan to tryptamine, which is similar to serotonin produced in the gut. Researchers in the lab found that tryptamine activates a receptor in a mouse gut that normally responds to serotonin and increases secretions in the intestine, resulting in faster movement of food. They engineered a bacteria to produce high levels of tryptamine in the intestine as a designer probiotic that could benefit patients who have constipation. This needs to be tested in humans.
“Bacterially produced tryptamine quickly degrades in the intestine and doesn’t appear to increase in the bloodstream,” says Dr. Kashyap. “Our goal is to find treatments that act only in the GI tract without creating problems in other parts of the body.”
Dr. Kashyap’s lab also is studying C. diff infection and how this bacteria manages to remain in the intestine, causing disease again and again. Dr. Kashyap is exploring the possibility that C. diff sticks to the intestine by forming a biofilm on its surface and evades antibiotic treat ment. His long-term goal is to develop new biomarkers and microbiota-targeted therapies to treat GI disorders.
“The next generation of probiotics may involve engineering bacteria to change the microbiome or influence its function, whether that’s producing large amounts of tryptamine or other molecules that affect GI function,” says Dr. Kashyap.
Advancing precision and predictive medicine in rheumatoid arthritis
Most patients who are diagnosed with rheumatoid arthritis respond to either the first or second line of drug therapies. However, some patients try multiple drugs without improve ment in their condition. It can take as long as two years of suffering, disease progression and expense before landing on a medication they respond to.
John Davis III, M.D., Division of Rheumatology at Mayo Clinic in Rochester, says that’s not tailoring the right drug to the right person early enough. Dr. Davis is a professor in the Mayo Clinic College of Medicine and Science.
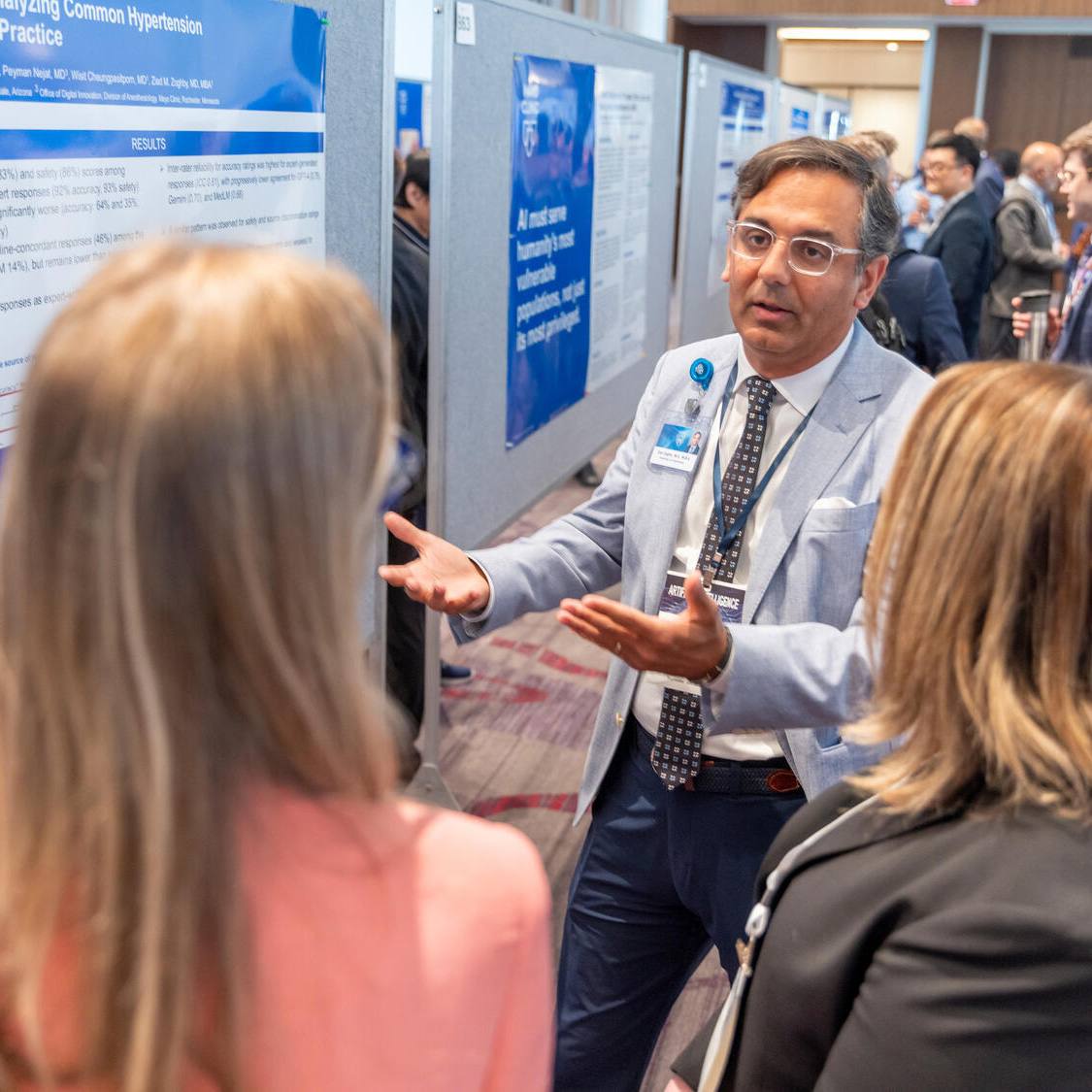
In an effort to shorten the interval to more effective treatment, Dr. Davis is studying the influence of the gut microbiome on the course of rheumatoid arthritis and response to treatment. His research aims to identify features in the microbiome that are associated with and predictive of changes in disease symptoms after therapy. A recent study on which he is co-senior author, published in Genome Medicine, found that the gut microbiome is indicative of whether or not patients will show minimum clinically important improvement in rheumatoid arthritis symptoms. It was the first study that used gut microbiome data to predict clinical improvement in rheumatoid arthritis disease activity independent of the patient’s condition or prior treatment.
“We’re trying to develop new biomarkers based on profiles of gut microbes that will enable us to predict who will respond to one drug versus another,” says Dr. Davis. “The gut microbiome is highly dynamic and reflective of a patient’s current state and history. The results of our exploratory study suggest that profiles based on the gut microbiome will tell better than any other clinical predictor how someone will do clinically in six to 12 months.”

Dr. Davis, his research collaborator Jaeyun Sung, Ph.D., Department of Surgery, co-senior author of the study and an assistant professor in the Mayo Clinic College of Medicine and Science, and their team performed a comprehensive genomic analysis on stool samples of patients with rheumatoid arthritis at two separate clinical visits. The team investigated the connection between the gut microbiome and the smallest meaningful changes in clinical disease activity and found several traits of the gut microbiome linked to prognosis.
“We observed significantly different microbiome traits between patients who eventually showed improvement and those who did not,” says Dr. Davis. “Using deep learning artificial intelligence (AI), we examined if we could predict whether a patient would achieve clinical improvement. The predictive performance resulted in 90% accuracy, demonstrating the proof of concept that the integration of gut microbiome and AI could be an avenue to predict disease course in rheumatoid arthritis.”
The researchers hope the biomarkers will inform precision medicine in the clinic. They envision a future state in which assessing the gut microbiome is a part of a patient’s workup, helping clinicians determine which medication to select. They also would like to develop a screening test to identify rheumatoid arthritis as early as possible.
Dr. Sung says the response to this research from the patients with rheumatoid arthritis, rheumatologists and scientific communities is one of the biggest he’s seen in his career. “We’re not yet ready to make an impact on the practice, but we’re on the path to advancing precision and predictive medicine — utilizing microbiome data and learning how to intervene on and impact the gut microbiome to improve chronic disease.”
Dr. Davis notes that their clinical findings, when combined with AI, may have a huge impact on the way treatment is delivered in the decades to come. “We expect our work to be a cornerstone for a new suite of omics data-based clinical tools to aid in the early detection, diagnosis, prognosis and treatment of rheumatoid arthritis.
“When a patient comes in with symptoms, we’ll be able to use all types of omics data to determine if they’re at risk for rheumatoid arthritis, which subtype of the condition they have if they have the disease, and predict when their condition will flare up, when they need to be seen by a physician and when we need to be aggressive with their treatment. This could revolutionize how we deliver care to patients. Much remains to be done, but we’re on the right path toward advancing our understanding of this disease and to individualizing medicine for patients.”
Identifying contributor to endometrial cancer
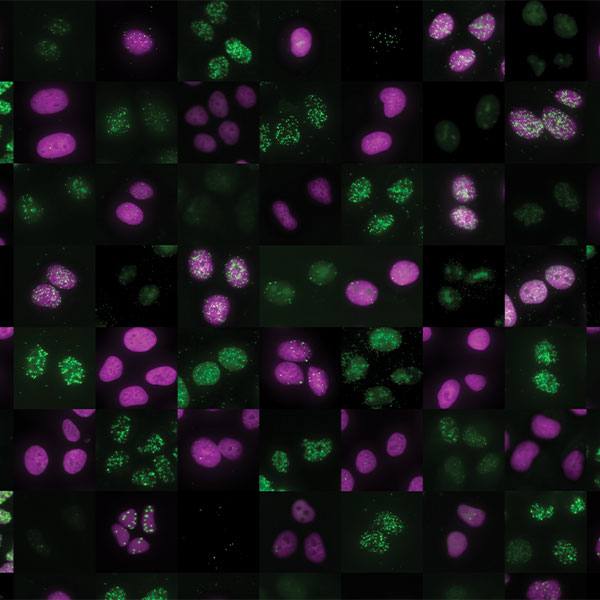
Marina Walther-Antonio, Ph.D., Departments of Surgery and Obstetrics and Gynecology at Mayo Clinic in Rochester, is a pioneer in studying the role of the microbiome in women’s health. Dr. Walther-Antonio is also Dean of Diversity, Equity and Inclusion in the Mayo Clinic Graduate School of Biomedical Science and an assistant professor in the Mayo Clinic College of Medicine and Science. She’s investigating the possibility that a microbe her team has identified in the vagina and uterus is a contributor to endometrial cancer. Most women don’t have this microbe, Porphyromonas somerae (P. somerae), in their vaginal or uterine microbiome. However, it is present in small amounts in 86% of women who have endometrial cancer.
Little research has been conducted about P. somerae. Several reports show it has been found in chronic bone and tissue infections of people who have diabetes. Dr. Walther-Antonio, a full-time faculty member in the Mayo Clinic Center for Individualized Medicine’s Microbiome Program, and her team are studying how this uncommon microorganism persists in the reproductive tract. They’ve completed three studies that link P. somerae to endometrial cancer.
P. somerae produces succinate, which can interfere with normal cellular functioning and accelerate cancer-causing pathways. P. somerae also is stimulated by estrogen exposure — a risk factor for endome trial cancer. One possibility Dr. Walther-Antonio’s team is investigating is that P. somerae invades endometrial cells in the uterus and produces succinate, compounding an individual’s risk.
Dr. Walther-Antonio and her team are the first to make this discovery, published in Frontiers in Microbiology. Now she wants to use this information to predict which women may develop cancer and find a way to intervene and prevent it.
“Our goal is to move the field beyond simple association and correlation and into proof of pathogenic behavior,” says Dr. Walther-Antonio. “This will be a significant leap toward understanding the role of the microbe in the disease and places us one step closer to identifying new therapeutic targets and being able to help patients.”
In addition to therapeutic targets, Dr. Walther-Antonio would like to develop a test for endometrial cancer, using this finding of P. somerae as an early-detection biomarker.
“Most endometrial cancer is detected early because it’s symptomatic, with vaginal bleeding,” she says. “More severe cases, however, don’t manifest that way, so aggressive cases often aren’t detected until later stages of the disease. Black women are more likely to have more aggressive cases as well as symptomatic fibroids, so they and their physicians may overlook bleeding as a concern.”
Dr. Walther-Antonio is planning work with Emory University and Johns Hopkins University to gain access to larger numbers of Black women for her research. She’s committed to addressing what she calls a serious public health problem with a disproportionate impact on minority populations.
“Endometrial cancer kills twice as many Black women as white women, making it the leading cancer-related health disparity in women in the U.S. The current test for endometrial cancer is an endometrial biopsy, which can be painful and expensive. We envision developing a vaginal swab test for endometrial cancer biomarkers that a woman could take at home and send to a laboratory for PCR testing. That’s the ultimate translation of our research — providing those at greatest risk with an easy-to-use predictive test so we can intervene and treat them with therapeutic agents to stop cancer in its tracks.”
Mapping all 22 feet of the small bowel microbiome
Is the microbiome of the small bowel different from that of the colon? No one knows. That’s because, until recent years, physicians could view only the top and bottom 10 to 20 centimeters, not the hundreds of centimeters in between. Thanks to balloon-assisted enteroscopy, physicians at specialized centers can now see the entire small bowel — all 22 feet of it.
That technology has opened the door for Kevin Ruff, M.D., Division of Gastroenterology and Hepatology at Mayo Clinic in Arizona, to investigate and map the microbiome of the small bowel. Dr. Ruff is also an assistant professor in the Mayo Clinic College of Medicine and Science. He’s taking samples from the length of the small bowel to determine if different areas of the organ have different microbiomes and how they correlate with the microbiome of stool samples.
He’s completed a small study for proof of concept and is pursuing funding to continue this work collect samples from deep in the small bowel from a larger number of patients.
“I see patients who need balloon-assisted enteroscopy because they have bleeding blood vessels in the small intestine that are difficult to reach,” says Dr. Ruff. “We don’t know why some people have this condition and others don’t. Perhaps something in the microbiome predisposes them to have a more sensitive intestinal lining that is prone to bleeding.
“Studying and mapping the small bowel microbiome will help us to classify a person’s microbiome and, we hope, prevent these obscure GI bleeds from occurring by modifying the microbiome with diet or medication to create better health outcomes. We’re in the early stages of understanding the significant impact on health and wellness that altering the microbiome could have. But we’re relatively certain it has a major impact on the body’s overall state of inflammation and neurologic and immunologic systems. My work to determine if a stool sample is a great representation of the entire length of the small bowel is one small step in improving our understanding of the microbiome.”
Exploring probiotics' role in decreasing cancer side effects and improving treatment response
Immune checkpoint inhibitors (ICIs) have revolutionized cancer treatment but can lead to gastrointestinal symptoms including colitis in as much as 45% of patients. Approximately 30% of those patients may need to discontinue this lifesaving therapy.
Patients who develop ICI-induced colitis typically have symptoms after the second or third dose of treatment. But histologic findings, including inflammation, may precede symptoms by as many as three weeks. Early recognition of ICI-induced colitis and timely treatment with immunosuppressant medication — and withholding ICIs — is important and improves outcomes.
Increasingly, evidence has demonstrated the relationship between the gut microbiome and response to immune checkpoint inhibitors. Early data also suggests an association between gut dysfunction and ICI-induced colitis. Saranya Chumsri, M.D., Division of Hematology and Medical Oncology at Mayo Clinic in Florida, and colleagues including the Division of Gastroenterology and Hepatology’s Francis (Frank) Farraye, M.D., and Maria Vazquez Roque, M.D., are conducting a pilot clinical trial of over-the-counter probiotics for cancer patients receiving immune checkpoint inhibitors as standard of care. Patients will be followed for six months during their ICI therapy. The researchers will analyze measures including hospitalization, dose reductions, treatment delays and use of immunosuppressant medication. They also will evaluate patients’ stool and blood samples for changes in the gut microbiome and immune status at baseline and at points during treatment to determine if the probiotics had an effect. The overall goal of the study is to evaluate the benefit of over-the-counter probiotics in preventing ICI-induced colitis. The results of the trial will provide a foundation for the development of larger randomized trials.
Dr. Chumsri and Dr. Farraye, are professors in the Mayo Clinic College of Medicine and Science; Dr. Vazquez Roque is an assistant professor.
“We can’t modify a person’s or tumor’s genetic makeup, but we may be able to re-engineer the microbiome with probiotics and diet to reduce the toxicity and side effects of cancer treatment,” says Dr. Chumsri.
In another research project, Dr. Chumsri is studying whether using probiotics to change the gut microbiome will alter a person’s immunological response to breast and lung cancers. Her team will examine patient stool, blood and tumor samples before and after taking probiotics. She hypothesizes that taking probiotics before surgery will significantly increase tumor-infiltrating lymphocytes, particularly cytotoxic T cells in tumors.
“We learn more about the association between microbiome diversity and cancer outcomes every day,” says Dr. Chumsri. “I hope one day we’ll be able to use probiotics and diet to augment traditional cancer treatment to enhance its effectiveness.”
Manipulating the gut bacteria and immune system in colorectal cancer
The colon claims the highest density of bacteria in the body. Those bacteria play an important role in the development of the GI tract and immune system.
Khashayarsha Khazaie, Ph.D., Department of Immunology, Mayo Clinic in Arizona, is exploring the relationship between the gut microbiota and the immune system and how, in colorectal cancer, this healthy balance becomes pathogenic. Dr. Khazaie is a professor in the Mayo Clinic College of Medicine and Science. The work is part of a long-standing scientific collaboration with colleague Foetini Gounari, Ph.D. A central focus of this study is the role of regulatory T cells. As their name suggests, these cells regulate immune responses, including to bacteria, injury and tumor growth. Change in the composition of gut bacteria alters immunity and vice versa. For example, tumor growth alters the gut microbiota, which then changes the immune system and can either promote tumor rejection or help the tumor grow and become more aggressive.
Dr. Khazaie studies how bacterial communities in the gut modulate immunity in colorectal cancer. Learning how harmful bacteria manipulate the immune system could inspire the development of effective targeted cancer therapies. This is important for malignancies that depend on bacteria for their initiation and progression, particularly colorectal cancer.
Dr. Khazaie examines the role of two classes of microbiota in intestinal carcinogenesis — oral microbiota that serve as opportunistic pathogens in colorectal cancers and bile acid-metabolizing bacteria that promote the generation of regulatory T cells in the gut.
A collaborative study with the University of Paris identified strains of oral microbiota that contribute to the risk of colorectal cancer by introducing epigenetic changes in the gut epithelial and blood cells. The idea is that these epigenetic changes are responsible for the shift of immunity from protective to pathogenic.
In another study with the University of Illinois Urbana–Champaign, Dr. Khazaie investigates how a minimal community of eight strains of bile acid-metabolizing bacteria determine T regulatory cell functions in the healthy versus tumor-bearing gut. The researchers found that colonization of germ-free mice generates regulatory T cells that protect the mice against the onset of tumor growth. However, after tumor onset, the composition of bacteria and regulatory T cell functions change to favor tumor growth. The team examines how bacteria-induced changes in T regulatory cells cause pathogenic immunity and tumor growth.
“If we can manipulate pathogenic immunity through microbiota or targeted drugs, we may be able to improve patient response to treatment, whether it’s the standard of care or immunotherapy,” says Dr. Khazaie.
“Cancer is a systemic disease. In the coming decade, cancer therapy will specifically target the underlying systemic mechanisms of the disease. The future will bring intelligent, personalized intervention."
This article was originally published in Alumni Magazine, 2022, issue 3.