
On the brink of losing her battle with acute myeloid leukemia, Shannon Camlek arrived at Mayo Clinic as a last hope. Her chances didn’t look good, but with the help of specialized genetic testing, particularly FISH (fluorescence in situ hybridization) studies, doctors were able to detect the specific gene mutations responsible for her symptoms and disease. The test results also helped Shannon’s care team target her treatment accordingly, and finally put an end to what Shannon likens as starring in her own personal horror movie while in search of hope and healing.
"Her white blood cell count was very high and there were all these leukemia cells (blasts) in her blood." This is how Naseema Gangat, M.B.B.S., a consultant in Mayo Clinic’s Division of Hematology, describes patient Shannon Camlek’s condition when she first arrived at Mayo Clinic’s Rochester campus. It was April of 2018, and Shannon had been diagnosed with acute myeloid leukemia (AML). Her condition had deteriorated so dramatically that Shannon’s care team at Sacred Heart Hospital in Eau Claire, Wisconsin, urged her to come to Mayo Clinic as a last-ditch effort to extend her life.

To determine the appropriate treatment for Shannon, Dr. Gangat ordered a second bone marrow biopsy, posthaste, after the first one was lost in transit from Sacred Heart. "I was not in good shape," says Shannon, 55, who resides in Fall Creek, Wisconsin, with her husband Tim. "My platelets were down, my white blood cell count up. I was in what they call ‘blast crisis,’ and the genetic tests from the bone marrow sample held the answers to my treatment plan. So, getting those results was a matter of life and death."
DR. GANGAT ADDS, “WE NEEDED THE BONE MARROW RESULTS TO ACCURATELY PROGNOSTICATE OR RISK-CLASSIFY THE DISEASE. IN SHANNON’S CASE, THE CHROMOSOME TESTS WERE NORMAL, BUT HER FISH STUDY, WHICH IS ANOTHER GENETIC TEST, REVEALED AN ABNORMALITY WITH THREE COPIES OF THIS GENE CALLED KAT6A, AND MUTATION ANALYSIS HAD THE FLT3-ITD MUTATION.”
The FISH (fluorescence in situ hybridization) study is a highly sensitive test done in Mayo Clinic’s Genomics Laboratory. The test performed on Shannon ran 16 different probe sets, including the gene region KAT6A, which is how the third copy of the mutation was discovered (the norm is two copies).
The FLT3-ITD mutation put Shannon’s leukemia in the high-risk category, which meant a stem cell transplant was her only viable treatment option. The presence of the FLT3-ITD mutation also provided the opportunity to use FLT3-directed medications. Foremost, given Shannon’s presentation with "blast crisis," Dr. Gangat ordered a leukapheresis, a procedure to remove white blood cells and help prevent organ damage. Shannon was then moved into an induction chemotherapy program consisting of cytarabine (7) + daunorubicin (3) plus.
"We performed disease assessment about a month after treatment was started," Dr. Gangat says. "And there still were about 4% of leukemia cells remaining, which we call ‘persistent AML.’ So, we did another round of the same treatment to enable the eradication of all leukemia cells. The stem cell transplant doesn't work as well if you go into it when disease is still present, because it means you are more likely to relapse."
A horror movie that won’t end
The second round of chemo meant even more risk to Shannon’s chances of survival. "I got real sick in that second round," she says. "I ended up in ICU with a lung hemorrhage. I got so bad we made plans for a funeral. I mean, it was like a horror movie. I look back and I think, ‘Was all this a dream? Did I really go through that and make it out the other side?’"
Once Shannon recovered from the second round of chemo and the ensuing complications, a donor was sought for her stem cell transplant. Siblings are often ideal candidates because there is a higher chance of matching more of the human leukocyte antigen (HLA) antigens — there are over 100 different types of these special white blood cells, which are part of the genetic makeup in each person’s immune system. A higher match of these antigens makes for a better engraftment of the donated bone marrow. Fortunately for Shannon, testing reveled her brother Pat to be a perfect match.

For this phase of her treatment, Shannon came under the care of Mithun Shah, M.D., Ph.D., a hematologist and consultant in Mayo’s Division of Hematology. A big fear for Dr. Shah was that Shannon might have recurrent bleeding in her lungs during the transplant procedure. To prepare for that possibility, he and his team had to make sure there was a source of donated blood ready if needed — and not just any blood, but HLA antibody platelets. "That makes it very difficult for us to just randomly select donors for these specific platelets," Dr. Shah says. "So, we had to talk to the transfusion team and make sure we had planned donors who would be ready to come in and donate on short notice."
In August of 2018, Shannon underwent a stem cell transplant at Mayo Clinic. It was a complete success. "We had to use very minimal transfusion support, which is quite remarkable and very rarely seen in transplant," Dr. Shah says. "And then, post-transplant, her counts recovered well, and Shannon came through it like a champ."
A relapse doesn’t always mean "game over"
Even so, about nine months after her transplant, Shannon relapsed. And this is where Mayo’s specialized FISH testing, again, helped inform and guide the next stage of her treatment.
"WE DID A BONE MARROW BIOPSY, NOT EXPECTING ANY PROBLEMS TO BE THERE," DR. SHAH SAYS. "BUT THEN WHEN WE RAN A MORE SPECIALIZED FLUORESCENCE IN SITU HYBRIDIZATION TEST, WE WERE ABLE TO SEE THAT LEUKEMIA CELLS HAD COME BACK. AND THAT WAS A UNIQUE PART OF HER STORY BECAUSE, USUALLY, WE DON'T HAVE TO RUN FISH TESTS FOR LEUKEMIA PATIENTS OVER AND OVER AGAIN. WE ARE USUALLY IN THE CYTOGENETICS LAB, AND THAT’S WHERE WE STOP. BUT IN SHANNON’S CASE, WE WENT FOR THE FISH STUDY WHERE THEY FOUND RELAPSE SOLELY BASED ON THAT TEST, MEANING HER LEUKEMIA WAS COMING BACK AT A VERY, VERY LOW LEVEL. SO THAT AGAIN INFORMED OUR DECISION TO COME DOWN ON IMMUNOSUPPRESSIVE MEDICATION."
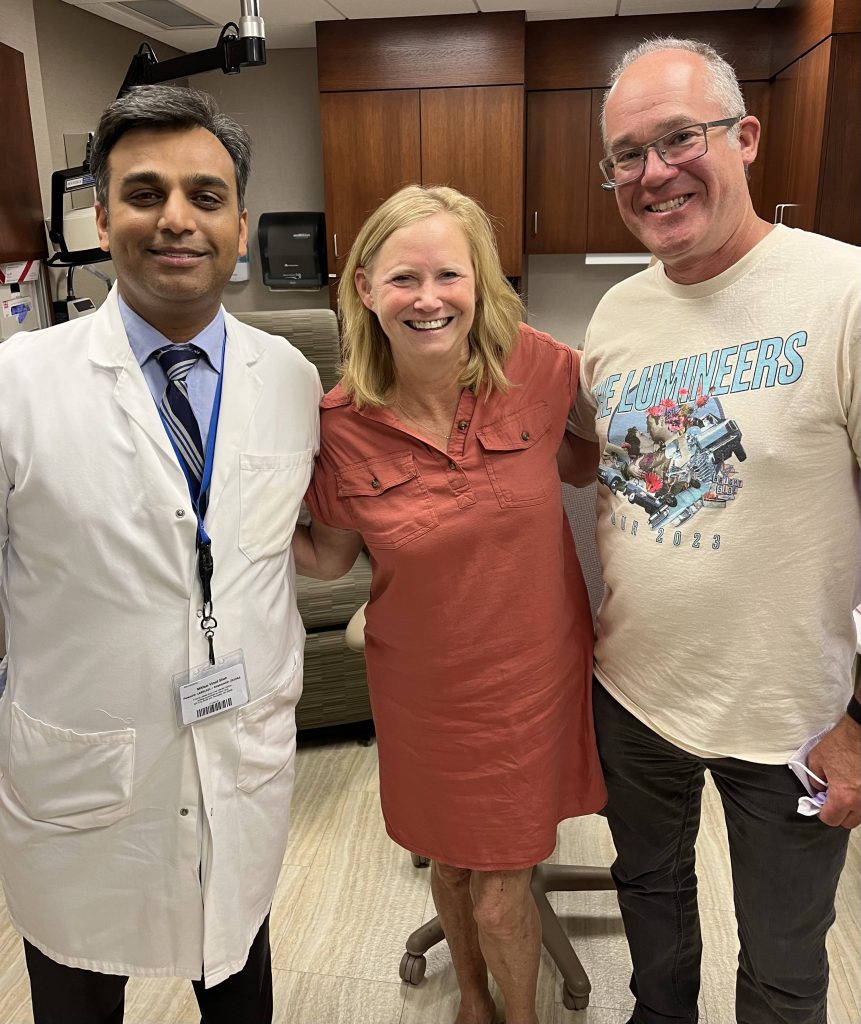
In accordance to the results of her testing, Shannon was put on targeted medication to address the leukemia cells that had returned to her body. After two years, however, she was able to discontinue the meds and has been in remission ever since. "I've been in remission for four years," she says. "My husband has been my rock through it all."
Both Shannon and Tim do not take lightly the role that the Genomics Lab and other labs at Mayo Clinic played in her treatment.
"THE PEOPLE DOING THE TESTING IN THE LABS HAVE ALWAYS BEEN AT THE HEART OF MY CARE," SHE SAYS. "IT STARTS WITH THEM. WE WERE AMAZED BY THE WORK THEY DO, AND WHAT HAPPENS BECAUSE OF THE WORK THEY DO. THE DOCTORS GET ALL THE GLORY AND THE PAIN. BUT WE SAW FIRSTHAND THAT IT’S WHAT HAPPENS AT THE CELLULAR LEVEL THAT REALLY DRIVES THIS ORGANIZATION AND PATIENT CARE."
Tim shares his wife’s appreciation for Mayo Clinic’s lab staff. "I’m a sixth-grade science teacher, and I was amazed by the amount of elementary, middle, and high school science that goes on inside a workplace like Mayo Clinic," he says. "And a theme that comes through in our narrative is those connections between the lab people, from a microscope and cellular level, on up to the doctors, and how that all works together. It’s changed how we look at medicine."
The lesser-known “cost” of long-term cancer treatment
In all, Shannon and Tim ended up shuttling from Wisconsin to Rochester for eight months to get through all her treatments and follow-ups. For five of those months, they needed to live on Mayo’s campus in downtown Rochester, but Shannon’s insurance didn’t cover the additional expense of housing. And because of her medical issues, she had to give up her beloved 28-year career as a schoolteacher (third and sixth grades). The financial strain caused additional stress they didn’t need during that time.
Because Shannon doesn’t want other cancer patients to have to go through the financial headaches and worries her family did over patient housing, she and a friend cofounded Home 4 Healing, an organization that helps make housing more affordable and accessible for patients whose treatment necessitates extended stays near the Mayo Clinic campus.
"Dr. Gangat has been a key inspiration in helping me start Home 4 Healing," Shannon says. "She actually said to me, ‘We need this. We need to be able to offer people a place to go when we tell them they have to be here for long periods of time.’"
Shannon, meanwhile, remains under the care of Dr. Shah, who is optimistic about her future. "We try not to use the word ‘cure’ for leukemia," he says. "But every time I meet with Shannon, I tell her the chances of the leukemia coming back get smaller and smaller the longer she’s in remission. So, for all practical purposes, we hope, and we think, that she may be cured."
This article first published on the Mayo Clinic Laboratories blog.







