-

How specialized blood cells could transform treatments for inflammatory disease

Mayo Clinic researchers are studying whether specialized T cells taken from blood could harness the body's immune system to treat or someday cure complex inflammatory diseases.
Researchers are probing whether a subset of T cells known as regulatory T cells, or Tregs, have the power to suppress out-of-control immune responses. If so, they want to know if this could offer a new therapeutic option for chronic inflammation that does not respond to standard treatment.
William Faubion, Jr., M.D., a gastroenterologist who is dean of Research at Mayo Clinic in Arizona and medical director of Mayo Clinic's Center for Regenerative Biotherapeutics is leading a team of researchers focused on the therapeutic value of Tregs for inflammatory bowel disease.
"While many new agents are emerging for the treatment of inflammatory bowel disease, unfortunately many patients still do not completely respond, leaving a huge unmet need,” says Dr. Faubion. "Tregs are master regulators that control the immune response through many mechanisms; thus, we are interested to learn if they could restore proper immune tolerance."
A new approach to cell therapy
The allure of Tregs lies in their potential to deliver healing messages to diseased tissues while sparing normal tissues. Dr. Faubion's team will study whether Tregs can be loaded with specific receptors to target intestinal inflammatory conditions and restore healthy immune function for patients. Preclinical studies have shown promising results, but engineered Tregs have not yet been studied in humans at Mayo Clinic. Exploring Tregs as a cellular therapy in clinical care would be a new approach for targeting the molecular underpinnings of inflammation and stopping it at its source.
"Many of the current anti-inflammatory medicines have negative side effects, such as infections," says Dr. Faubion. "New solutions are needed. Our hope is to understand whether Treg cell therapy could control symptoms, minimize the risks and be a more convenient form of treatment than currently exists for chronic inflammation."
Cellular mechanisms in action
T cells are a type of white blood cell that act as beacons of protection, triggering the immune system to block viruses, bacteria and abnormal cells that cause disease. However, an "off target" effect of T cells can shift the body's inflammatory system into overdrive and cause it to mistakenly attack healthy tissue. The result can be autoimmune disorders such as psoriasis, rheumatoid arthritis and inflammatory bowel diseases like ulcerative colitis and Crohn's disease.
Approximately 8% of people in the U.S. have an autoimmune disease, according to the National Institutes of Health. Standard therapies can sometimes ease the symptoms but are not a cure.
Tregs, derived from T cells, act as gatekeepers of the immune system. They release anti-inflammatory molecules and growth factors to control the body's immune response. They also prevent new T cells from activating, while recruiting other immune cells to promote a calming, immune-tolerance environment that could control or stop inflammatory disorders.
Biomanufacturing Tregs for inflammatory disease
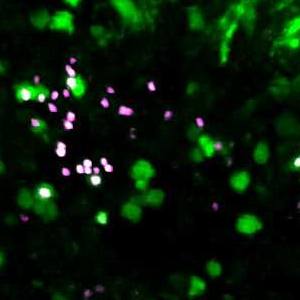
To better understand the clinical potential of these specialized cells, researchers take Tregs from a patient's blood and then modify them for use in clinical trials. The Center for Regenerative Biotherapeutics is engineering these cells and establishing a process for isolation, expansion and biomanufacturing. The goal is to ensure the cells meet safety and quality standards for patients in clinical trials.
"On-site facilities at Mayo Clinic allow us to begin the biomanufacturing process without delays and limit the risks to biological integrity that can come with shipping," says Julie Allickson, Ph.D., the Michael S. and Mary Sue Shannon Director of the Mayo Clinic Center for Regenerative Biotherapeutics. "We are excited about the prospect of offering Tregs as an experimental cell therapy that is studied in clinical trials for patients with complex inflammatory diseases."
Dr. Allickson is also the Otto Bremer Trust Director, Biomanufacturing and Product Development, Center for Regenerative Biotherapeutics.
A better understanding of Tregs on a molecular level could have clinical value. Mayo Clinic research teams in Arizona are poised to lead this research in collaboration with colleagues in Rochester and Florida.
Dr. Faubion's team hopes to obtain regulatory approval for clinical trials to study Tregs in patients with inflammatory bowel disease by the fourth quarter of 2024.
####
Related articles:
Growing mini organs to find new treatments for complex disease
Early Mayo Clinic research finds hope in stem cell therapy for perianal fistulas