-
Research
Brain stimulation shows promise in treating drug addiction
Today, neurostimulation is used to treat a variety of human disorders, including Parkinson's disease, tremor, obsessive-compulsive disorder and Tourette syndrome. A Mayo Clinic neurosurgeon and his colleagues believe one form of that treatment, called deep brain stimulation (DBS), is poised to solve one of the greatest public health challenges: drug addiction.

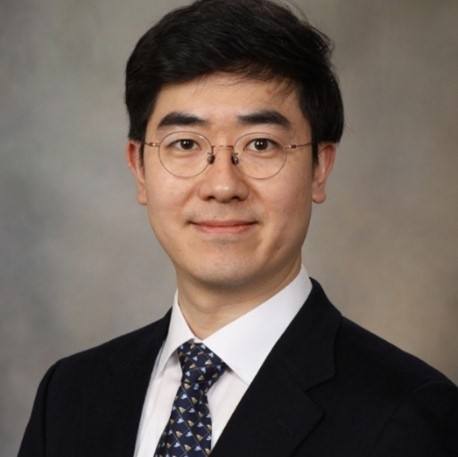
"Drug addiction is a huge, unmet medical need," says Kendall Lee, M.D., Ph.D., who has published nearly 100 journal articles on DBS along with his colleagues. Key to treating it, he says, is cutting off the pleasurable "high" that comes with the addiction — which DBS potentially can do.
"We now have several early studies showing promise in suppressing the rapid increase in dopamine that makes people feel high," he says.
Rethinking reward
In 2023, a record 112,000 people in the U.S. died after overdosing on drugs, including illicit drugs and prescription opioids. Even though several psychological and pharmaceutical treatments are available for addiction, as many as 75% to 98% of patients relapse.
"What's unique about addiction is it creates a pattern in the brain that is self-perpetuating. Essentially, the behavior reinforces itself, making it very resistant to intervention," says Mayo Clinic addiction psychiatrist Tyler Oesterle, M.D.
The brain is wired to make pleasure a priority. The brain’s reward system connects two tiny regions: the ventral tegmental area, which releases the feel-good chemical dopamine, and the nucleus accumbens, which controls memory and behavior. The former is why you feel a jolt of pleasure after biting into a hamburger. The latter is why your mouth waters whenever you smell someone fire up a grill. Drugs can overload this system, flooding it with dopamine and strengthening the connections that undergird addiction.
But what if you could short-circuit the reward system? If drugs no longer triggered a high, would they be easier to stop using? Preliminary research in animal models and humans suggests that it is possible to curtail drug-seeking behavior by electrically stimulating brain regions associated with reward.
"The results are promising, but we still don’t know how it works," says Mayo Clinic biomedical engineer Hojin Shin, Ph.D. "What we really need is a technique that allows us to see how the brain works and how the brain changes in response to stimulation so we can use that information to improve the treatment."
A dopamine sensor
As part of the Mayo Clinic Neural Engineering Laboratory, Dr. Shin and his colleague Yoonbae Oh, Ph.D., have been busy devising novel techniques to measure brain chemicals — such as dopamine and serotonin — in real time. The most recent iterations use electrodes composed of flexible carbon fibers thinner than a human hair, wirelessly connected to an electronic circuit that can simultaneously stimulate neurons and detect neurochemicals.

The researchers have used their innovations to glean important insights into the mechanisms of DBS and addiction in a preclinical study. The experimental DBS treatment cut the flow of dopamine to the nucleus accumbens, the brain’s reward center, by nearly half.
In another study, the team tested the approach on a rodent model of opioid addiction. When they gave the models a powerful opioid, they saw a spike in dopamine levels. But when they treated the models with DBS before administering the drug, that spike never happened. The experimental treatment also appeared to inhibit respiratory depression, the breathing difficulties responsible for the majority of opioid overdose deaths.

The team recently received a grant from the National Institutes of Health to obtain approval for an FDA Investigational Device Exemption, a necessary step for future preclinical studies and clinical trials of this experimental treatment.
"To see addiction as a biological problem, and to address it with biological treatments like this, is a paradigm shift," says Dr. Oesterle. "We know that the standard behavioral or pharmaceutical interventions don't work for everybody. We're pushing the envelope here because we know we need to do something different, truly different, to help people rebuild their lives."
The researchers associated with this project have a financial interest in the technology referenced in this story. Review the studies for a complete list of authors, disclosures and funding.







