-
8 innovations in neuroscience and brain research at Mayo Clinic
The brain is a critical, complex organ and intricate diseases affect it. Mayo Clinic researchers are leading discoveries into many conditions, including cancer, Alzheimer's disease and other forms of dementia, as well as how the brain fundamentally works. Eight research advancements led by neuroscience experts include:

Researchers discover new molecular drug targets for progressive neurological disorder
Progressive supranuclear palsy (PSP) is an uncurable brain disorder marked by walking and balance difficulties. Its symptoms mimic Parkinson's disease and dementia. Mayo researchers and collaborators have outlined new therapeutic targets that may lead to future treatments for PSP as well as Alzheimer's disease and related disorders.
"This research enhances our understanding of progressive supranuclear palsy and other related, incurable neurological disorders," says the study's senior author, Nilufer Ertekin-Taner, M.D., Ph.D., a Mayo Clinic neurologist and neuroscientist. "Moving forward, we can target these specific genes or others that are biologically related to them to develop a potential treatment for this untreatable disease."
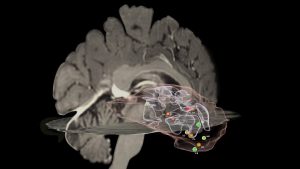
Mapping cell behaviors in high-grade glioma to improve treatment
High-grade gliomas are cancerous tumors that spread quickly in the brain or spinal cord. Mayo Clinic researchers found invasive brain tumor margins of high-grade glioma contain biologically distinct genetic and molecular alterations that indicate aggressive behavior and disease recurrence. They also found that MRI techniques, such as dynamic susceptibility contrast and diffusion tensor imaging, can help distinguish between the genetic and molecular alterations of invasive tumors, which is important for clinically characterizing areas that are difficult to surgically biopsy.
"We need to understand what is driving tumor progression," says lead author Leland Hu, M.D., a neuroradiologist at Mayo Clinic. "Our results demonstrate an expanded role of advanced MRI for clinical decision-making for high-grade glioma."

Researchers identify new criteria to detect rapidly progressive dementia
Rapidly progressive dementia (RPD) is caused by several disorders that quickly impair intellectual functioning and interfere with normal activities and relationships. If patients' symptoms appear suddenly causing rapid decline, a physician may diagnose RPD. These patients can progress from initial symptoms of dementia to complete incapacitation, requiring full-time care, in less than two years. Mayo Clinic researchers have identified new scoring criteria allowing for the detection of treatable forms of RPD with reasonably high confidence during a patient's first clinical visit. This scoring criteria may allow physicians to substantially reduce the time it takes to begin treatment.
"Many conditions that cause rapidly progressive dementia can be treated and even reversed. We found that more than half of the patients in our study with rapidly progressive dementia had a treatable underlying condition. We may be able to identify many of these patients early in the symptomatic course by intentionally searching for key clinical symptoms and exam findings and integrating these with results of a brain MRI and spinal tap," says the study's senior author, Gregg Day, M.D., a clinical researcher at Mayo Clinic.

Global consortium to study Pick’s disease, rare form of early-onset dementia
Pick's disease, a neurodegenerative disease of unknown genetic origin, is a rare type of frontotemporal dementia that affects people under the age of 65. The condition causes changes in personality, behavior and sometimes language impairment. In patients with the disease, tau proteins build up and form abnormal clumps called Pick bodies, which restrict nutrients to the brain and cause neurodegeneration. Researchers at Mayo Clinic and collaborators worldwide have established the Pick's Disease International Consortium to study a specific MAPT gene variation known as MAPT H2 that makes the tau protein and acts as a driver of disease. They investigated a connection between the gene and disease risk, age at onset and duration of Pick's disease.
"We found that the MAPT H2 genetic variant is associated with an increased risk of Pick's disease in people of European descent," says Owen Ross, Ph.D., a Mayo Clinic neuroscientist and senior author of the paper. "We were only able to determine that because of the global consortium, which greatly increased the sample size of pathology cases to study Pick's disease."

Moments of clarity in the fog of dementia
Researchers define lucid episodes as unexpected, spontaneous, meaningful and relevant communication from a person who is assumed to have permanently lost the capacity for coherent interactions, either verbally or through gestures and actions. A study surveyed family caregivers of people living with dementia and asked them about witnessing lucid episodes.
"We have found in our research and stories from caregivers that these kinds of episodes change how they interact with and support their loved ones — usually for the better," says lead author Joan Griffin, Ph.D. "These episodes can serve as reminders that caregiving is challenging, but we can always try to care with a little more humanity and grace."
Untangling the threads of early-onset dementia
Changes in personality, behavior and language are hallmarks of frontotemporal dementia (FTD), the most common form of dementia in patients under the age of 65. New research provides insight into the role a specific gene and the protein it produces play in the development and progression of FTD, which is associated with degeneration of the frontal and temporal lobes of the brain. The researchers think the key may lie in the formation of fibrils, or tiny fiber-like structures produced by part of this protein, that sometimes get tangled up in the brain.
"We also think that these fibrils could one day serve as biomarkers to help clinicians determine FTD prognosis or severity, " says Jordan Marks, an M.D.–Ph.D. student with the Mayo Clinic Graduate School of Biomedical Sciences.

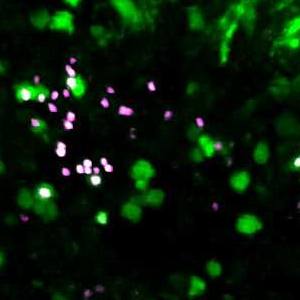
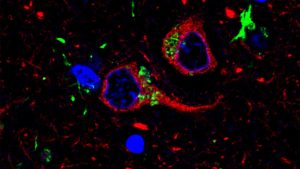
Mayo Clinic researchers' new tool links Alzheimer's disease types to rate of cognitive decline
Through a new corticolimbic index tool that identifies changes in specific areas of the brain, Mayo Clinic researchers discovered a series of brain changes characterized by unique clinical features and immune cell behaviors for Alzheimer's disease, a leading cause of dementia.
"By combining our expertise in the fields of neuropathology, biostatistics, neuroscience, neuroimaging and neurology to address Alzheimer's disease from all angles, we've made significant strides in understanding how it affects the brain," says Melissa E. Murray, Ph.D., a translational neuropathologist at Mayo Clinic. "The corticolimbic index is a score that could encourage a paradigm shift toward understanding the individuality of this complex disease and broaden our perspective. This study marks a significant step toward personalized care, offering hope for more effective future therapies."
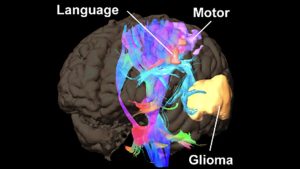
New research platform assesses brain cancer mutations during surgery
Brain cancer is difficult to treat when it starts growing, and a prevalent type, known as a glioma, has a poor five-year survival rate. Mayo Clinic researchers report on a new surgical platform used during surgery that informs critical decision-making about tumor treatment within minutes. Time is of the utmost importance when dealing with aggressive malignant tumors.
The researchers say that, in addition to enabling real-time diagnosis, the platform allows surgeons to determine a patient's prognosis and perform tumor resection to improve patient outcomes.
“We will be able to bring the fight against cancer to the operating room, before chemotherapy and radiation treatments begin, and before the disease has progressed and invaded further," says the study's senior author, Alfredo Quiñones-Hinojosa, M.D.