-
Mayo researchers study stool to unlock microbiome’s role in cancer treatment
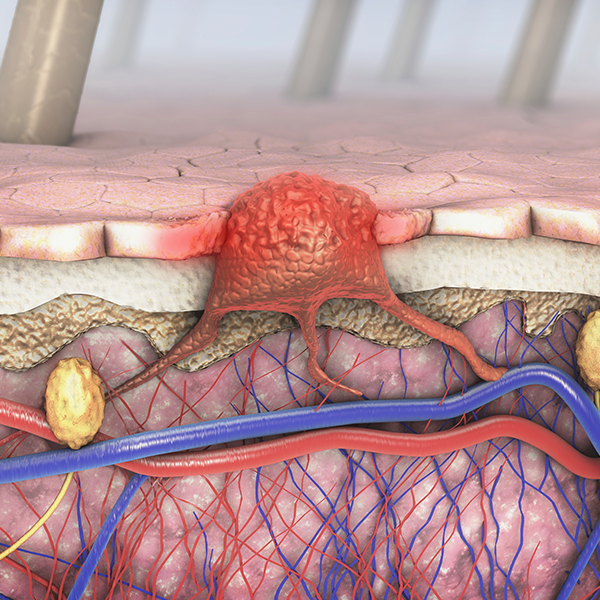
At Mayo Clinic’s Center for Individualized Medicine, scientists are investigating stool samples to uncover new insights into cancer treatment. Often seen as waste, stool may provide valuable information about the microbiome — a complex ecosystem of microorganisms, including bacteria, fungi and viruses in the gut.
Growing evidence shows the microbiome plays a significant role in health, including how the body responds to diseases like cancer and how it influences treatment outcomes.
A new frontier in cancer research

A key part of the team's research is the Oncobiome Project, an initiative within the center’s Microbiomics Program. The project includes a large collection of stool samples from patients with cancer across Mayo Clinic campuses in Minnesota, Arizona and Florida. These samples, collected before patients began treatment, are helping researchers identify microbial patterns that predict how well a patient will respond to treatments, and potentially pave the way for more personalized cancer care strategies.
What sets the Oncobiome project apart is its strategic design, which bridges research and clinical practice. This approach makes it easier to translate scientific discoveries into personalized treatments for cancer patients.
"Ultimately, we hope to individualize treatment plans that provide the right drug at the right time based on a person’s unique microbiome and genetics," says Purna Kashyap, M.B.B.S., the Bernard and Edith Waterman Director of the Mayo Clinic Microbiomics Program.
Decoding microbiome's cancer link through stool analysis

At the heart of the project is the collection and analysis of more than 2,000 stool samples. This extensive biobank allows Dr. Kashyap and his team to examine whether the microbiome composition correlates with specific types of cancer. They also are investigating whether the microbiome can predict the likelihood of event-free survival for patients with cancers such as lymphoma who are undergoing various treatments.
Additionally, the project explores whether enzymes and metabolites produced by the gut microbiome can offer insights into how patients will respond to cancer immunotherapies and help identify potential adverse reactions.

"We included a diverse group of patients at various stages of different cancers and undergoing various treatments. This allows us to identify microbial patterns that forecast optimal cancer outcomes, independent of the underlying cancer," Dr. Kashyap says.
Beyond personalizing cancer care, the team is integrating additional "omics" to gain deeper insights into patients' genetics, environment and immune status. This includes genomics (the study of genes), proteomics (proteins), exposomics (environmental exposures), metabolomics (metabolic processes) and transcriptomics (RNA transcripts).
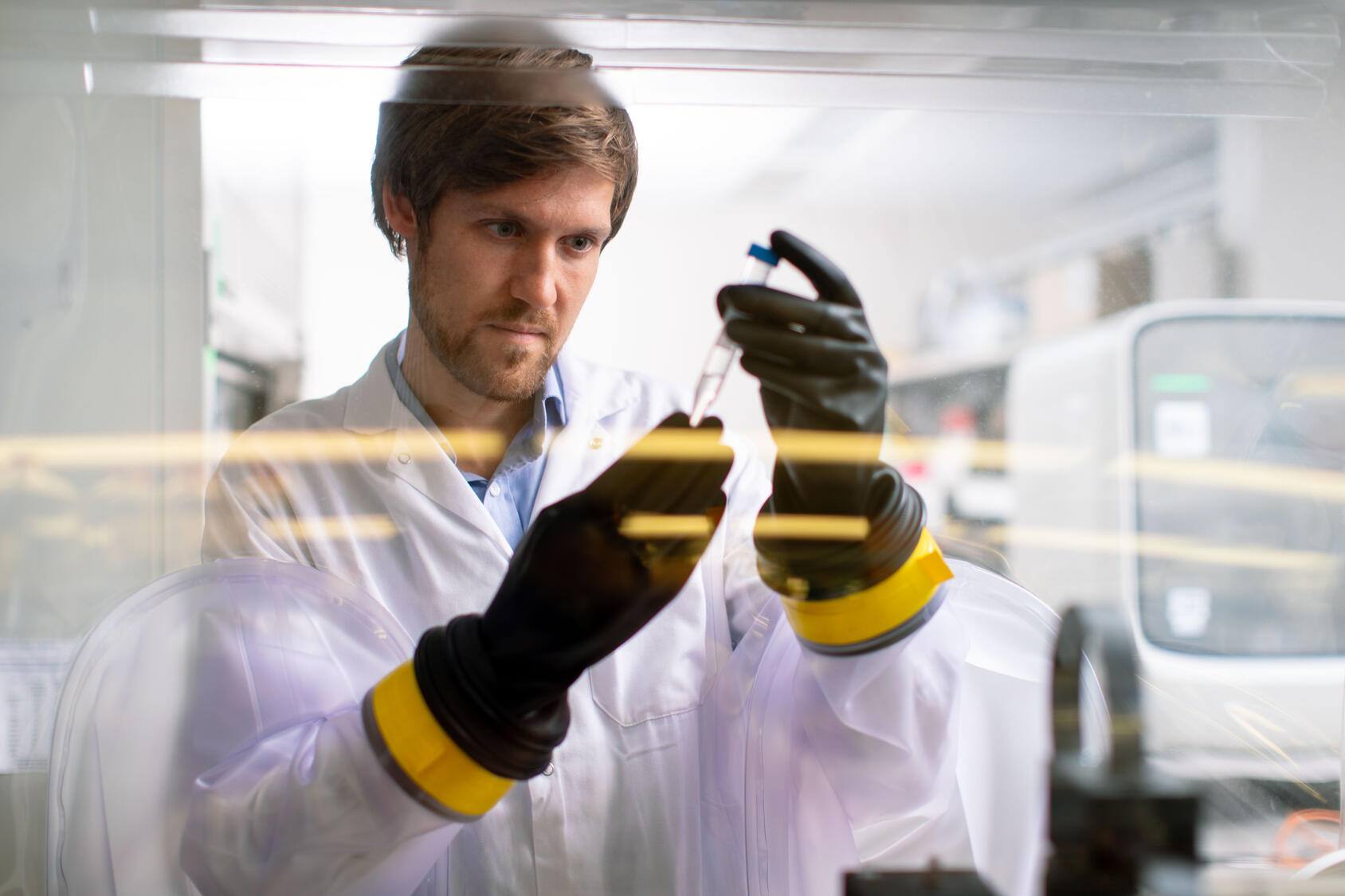
Ruben Mars, Ph.D., a research scientist at the Center for Individualized Medicine, is playing a key role in spearheading several studies within the Oncobiome project to understand the impact of microbes on cancer risk, treatment efficacy and the underlying mechanisms of any treatment side effects.
"Although a diverse and balanced gut microbiome is widely recognized as beneficial for our health, pinpointing specific microbial changes that enhance treatment outcomes remains challenging," Dr. Mars says. "Through the Oncobiome project, we're optimistic about developing innovative methods to manipulate the microbiome and ultimately improve cancer care for patients."

Connecting the microbiome to health outcomes
This research is part of a broader series of the team's investigations into the microbiome. Their recent published studies focus on the microbiome's role in gut-brain disorders, including how bacteria affect intestinal functions like motility. Other published work examines C. difficile infections, exploring how the bacteria persist in the intestine.
Mayo's microbiome scientists are also studying the impact of the gut microbiome on the progression of rheumatoid arthritis and patients' response to treatment. In another study, the team linked a specific microbe, Porphyromonas somerae, to endometrial cancer, finding its intracellular activity may play a pathogenic role in the disease.