-
Mayo Clinic Q and A: Leg pain? It may be your arteries

DEAR MAYO CLINIC: I'm 52 years old and enjoy long walks with my husband and our dog. I recently started to experience pain in my left calf during our walks. The leg pain goes away when I rest. Because I have a history of high blood pressure, I went to see my primary care physician and was diagnosed with peripheral artery disease. What is this condition, and what treatments are available? Will I need surgery?
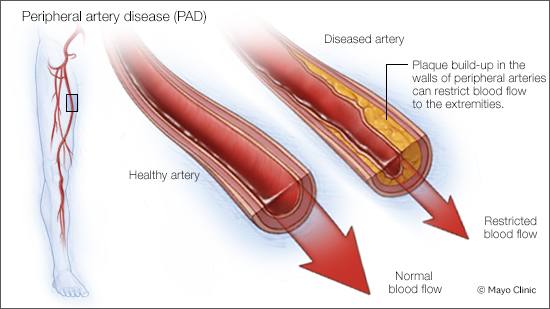
ANSWER: Peripheral artery disease is a common, chronic medical condition that affects circulation in the body due to narrowed arteries. The narrowing of arteries is caused by a buildup of fatty deposits, called plaque, which reduces blood flow from the heart to different regions of the body. This can affect the arms, but most commonly, it is an issue found in the legs.
The risk of developing peripheral artery disease increases with age, particularly for those over 65 or after 50 if you have certain risk factors. Factors that can contribute to your risk include:
- A family history of peripheral artery disease, heart disease or stroke
- High blood pressure
- High cholesterol
- Diabetes
- Chronic kidney disease
- Obesity (a body mass index over 30)
- Smoking tobacco/using tobacco products
Many people with peripheral artery disease have mild or no symptoms, while others experience leg pain when walking or even at rest. The severity of your symptoms and the extent of the blockage are used to categorize the stage of your peripheral artery disease and inform specific treatment options.
There are two stages of peripheral artery disease. The early stage is called claudication, when people experience pain when walking or engaging in activity. In this stage, the pain begins during exercise and ends with rest. It is usually felt in the calves, thighs and buttocks.
The advanced, severe stage of peripheral artery disease is called critical limb threatening ischemia. During this stage, pain is often felt in the feet, even without walking, and is worse during rest or when lying down. You also may experience open sores or wounds on your limbs or feet that won't heal. Critical limb threatening ischemia may cause tissue death or gangrene on your feet. If this goes untreated, it can lead to leg amputation.
Treatment for peripheral artery disease varies depending on its severity. When it's diagnosed early, lifestyle changes and treatment of underlying medical conditions are often enough to manage symptoms. This may mean taking appropriate medications to control high blood pressure and high cholesterol, controlling blood sugar levels if you have diabetes, quitting smoking, eating a healthier diet with fewer fatty and highly processed foods, and regular exercise or engaging in a walking program.
For more advanced disease, restoration of blood flow is necessary in addition to lifestyle changes. Therefore, the goal of surgery is to restore blood flow and prevent leg amputation.
One treatment option is percutaneous endovascular surgery, a minimally invasive approach. In this operation, the surgeon guides a thin, flexible tube called a catheter through the groin, foot or wrist to the narrowed part of the artery. A tiny balloon is inflated to widen the blocked artery and improve blood flow. A stent, a small wire mesh tube, may also be placed in the artery to keep it open.
The more invasive surgical option is bypass surgery. The surgeon creates a path around the blocked artery using either a healthy blood vessel from another part of the body or a synthetic one. One end of the healthy vein is connected to the artery above the blockage, and the other is attached below the blockage so that the blood will detour into the bypass.
When diagnosed with peripheral artery disease, it’s important to consult a vascular surgeon to determine the best treatment for you. Vascular surgeons can perform both minimally invasive procedures and complex bypass surgery.
By incorporating lifestyle changes and treating any underlying medical conditions early, you can significantly improve your quality of life and prevent progression to more severe stages of disease. Peripheral artery disease is a marker for your overall cardiovascular health, and managing it correctly can lead to a longer, healthier life. — Fahad Shuja, M.B.B.S., Vascular Surgery, Mayo Clinic, Rochester, Minnesota







