-
Cancer
New genomic test could spare some people with melanoma from lymph node biopsy surgery
ROCHESTER, Minn. — A genomic test co-developed by Mayo Clinic and SkylineDx can identify whether people with melanoma are at low or high risk for cancer in their lymph nodes — a finding that could guide treatment decisions and help some people avoid lymph node biopsy surgery. The study results are published in JAMA Surgery.
In the largest prospective study of its kind, about 93% of people classified as low risk had no cancer in their lymph nodes, while about 25% in the high-risk group did. The multicenter clinical trial enrolled 1,761 people with early- or intermediate-stage melanoma at nine U.S. cancer centers between 2021 and 2024.
Decoding the tumor’s genomic blueprint
The test measures the activity of eight genes in a melanoma tumor and combines that data with a person's age and tumor thickness to estimate the chance that cancer has reached the lymph nodes. The Merlin CP-GEP Test analyzes tissue from the tumor already collected during an initial biopsy, so no additional procedure or visit is required for the test.
Sentinel lymph node biopsy is performed under anesthesia to remove one or a few lymph nodes and check for microscopic cancer. The procedure usually requires a second incision and can have side effects, yet nearly 80% of people who undergo the surgery have no cancer in their lymph nodes.
"Surgery will always be central to cancer care, but this study shows that sentinel lymph node surgery might be avoided for selected patients with melanoma," says first author Tina Hieken, M.D., a surgical oncologist at the Mayo Clinic Comprehensive Cancer Center and co-principal investigator of the study. "This test lets us use a patient's own tumor biology to guide care with true precision."
Turning molecular insight into clinical impact
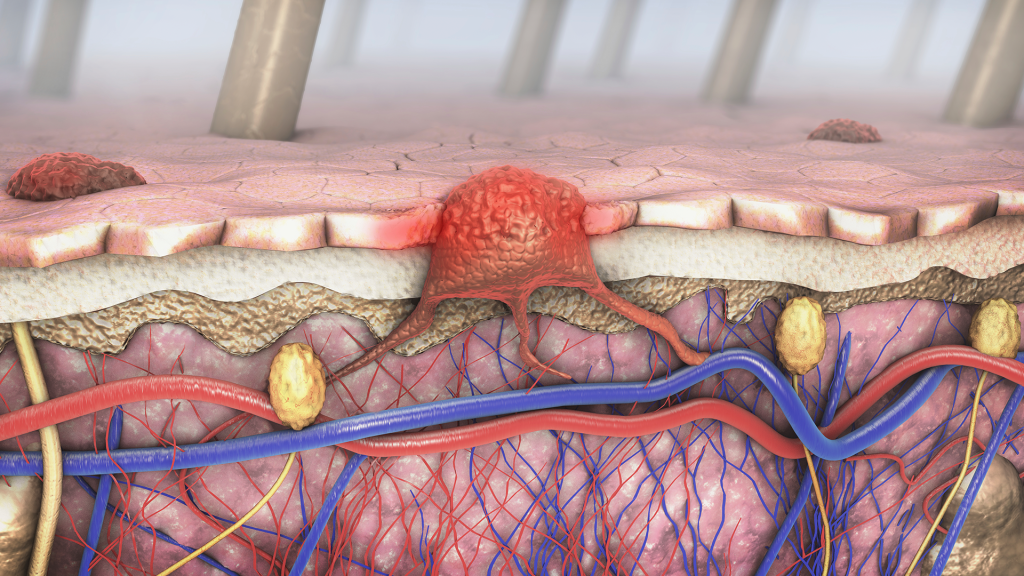
Melanoma is the deadliest form of skin cancer. While early-stage disease can often be treated successfully, once melanoma spreads to the lymph nodes, the risk of recurrence increases. Determining whether the cancer has reached the lymph nodes is a key step in guiding treatment.
"Melanoma progression is driven by subtle molecular processes that we're only beginning to understand," says Alexander Meves, M.D., a dermatologist at the Mayo Clinic Comprehensive Cancer Center who led earlier validation studies of the test. "This work translates that biology into tools that can improve care."
Researchers are now studying how incorporating the test into melanoma care might help healthcare professionals understand the risk of recurrence and guide follow-up care.
For a complete list of authors, disclosures and funding information, review the study.
###
About Mayo Clinic Comprehensive Cancer Center
Designated as a comprehensive cancer center by the National Cancer Institute, Mayo Clinic Comprehensive Cancer Center is defining the cancer center of the future, focused on delivering the world's most exceptional patient-centered cancer care for everyone. At Mayo Clinic Comprehensive Cancer Center, a culture of innovation and collaboration is driving research breakthroughs in cancer detection, prevention and treatment to change lives.
About Mayo Clinic
Mayo Clinic is a nonprofit organization committed to innovation in clinical practice, education and research, and providing compassion, expertise and answers to everyone who needs healing. Visit the Mayo Clinic News Network for additional Mayo Clinic news.
Media contact:
- Julie Ferris-Tillman, Ph.D., Mayo Clinic Communications, newsbureau@mayo.edu







