-
Mayo Clinic study sheds light on colorectal cancer risk in overlooked group

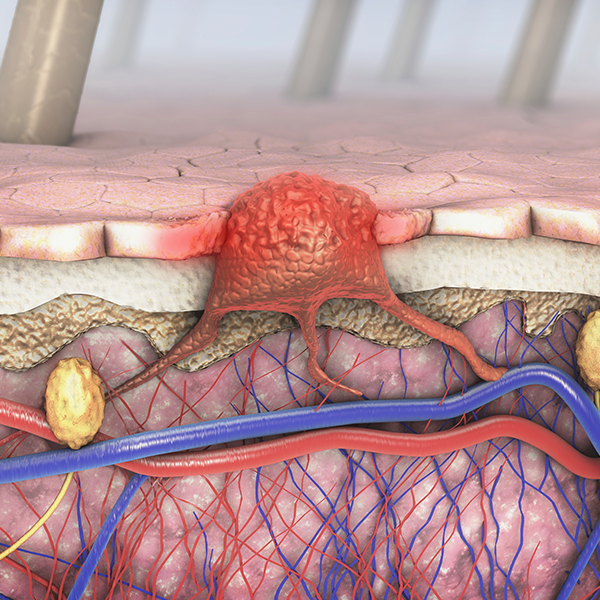
Primary sclerosing cholangitis (PSC) causes inflammation and scarring of the bile ducts. This rare liver disease is often accompanied by inflammatory bowel disease (IBD). Together, these diseases increase the risk of colorectal cancer by more than sixfold compared to the general population.
Until recently, it wasn't clear whether that increased colorectal cancer risk extended to people with PSC alone, but Mayo Clinic researchers have helped answer this question. Their findings could help open the door to earlier colorectal cancer screening and better prevention for people with PSC.

"We wanted to answer something that was overlooked in the guidelines because these patients are a smaller group and have been understudied in research," says Dr. Saqr Alsakarneh, a fellow in the Department of Gastroenterology at Mayo Clinic and lead author of the study, published in Alimentary Pharmacology and Therapeutics.
Searching data for cancer prevention blind spots
In the largest population-based analysis of its kind, Dr. Alsakarneh and his co-authors analyzed data from 115 million de-identified health records from 65 healthcare organizations across the U.S. Their goal was to understand long-term risk of colorectal and other gastrointestinal cancers in people with PSC.
The researchers found that people with PSC without IBD have nearly three times the risk of developing colorectal cancer compared to the general population.
"This is important because it challenges the current assumption that only primary sclerosing cholangitis with IBD causes colorectal cancer," says Dr. Alsakarneh.
While colorectal cancer prevention guidelines recommend annual screening and increased surveillance for people who have PSC and IBD, no specific guidelines exist for people with only PSC. Dr. Alsakarneh says this is a missed opportunity for early detection of colorectal cancer, which is highly preventable with proper screening.
In addition to discovering an increased risk for colorectal cancer, the study confirmed an association between PSC alone and higher rates of bile duct, liver and pancreatic cancers. While previous research has suggested this connection, the study provides large-scale data to support the need for continued vigilance and screening strategies tailored to people with PSC.
Translating discovery to better care
Dr. Alsakarneh says these findings are an important first step toward a better understanding of PSC and cancer risk, although more studies are needed to confirm how this information should be incorporated into healthcare guidelines.
"Before anything is put into guidelines, the first step is always to validate the findings," says Dr. Alsakarneh. "Colleagues from the gastrointestinal community have reached out and are interested, so this is something we are working on."
As researchers investigate further, Dr. Alsakarneh says it's important that clinicians with PSC patients be aware of this association, tune into emerging evidence and keep their patients informed as findings develop.
Continuing a legacy of PSC discovery at Mayo Clinic
Dr. Alsakarneh's research continues a legacy of PSC discovery at Mayo Clinic that dates back to the '70s. That was when Dr. Nicholas LaRusso, a gastroenterologist at Mayo Clinic, first began studying the cluster of symptoms that he eventually helped describe and define as PSC in a 1980 study.

"It's important to me that this study comes from Mayo Clinic because Dr. LaRusso, who still has a lab here, made so much progress in this disease. He is the reason I came to Mayo Clinic to do my training," says Dr. Alsakarneh.
Alongside Dr. LaRusso, Dr. Alsakarneh next plans to lead Mayo Clinic research investigating why and how PSC increases cancer risk.
Review the study for a complete list of authors, disclosures and funding.