-
Health & Wellness
Weekend Wellness: Communicate With Provider for Effective Plan Treating Depression
DEAR MAYO CLINIC: How soon after starting on antidepressants should I begin to feel better? What type of changes will I notice? It has been three weeks and I don’t feel like my depression has lessened. If anything, it seems to be getting worse. Do I need to try another medication?
 ANSWER: Many people who start taking an antidepressant begin to see some improvement in their symptoms within several weeks. But for others, it may take longer. The changes are not immediate or sudden, so you may not notice them much at first. Because of that, it is important to give the medicine time to work. Anytime you feel symptoms of depression getting worse, however, contact your health care provider.
ANSWER: Many people who start taking an antidepressant begin to see some improvement in their symptoms within several weeks. But for others, it may take longer. The changes are not immediate or sudden, so you may not notice them much at first. Because of that, it is important to give the medicine time to work. Anytime you feel symptoms of depression getting worse, however, contact your health care provider.
As with all medications, you need to take an antidepressant at an adequate dose for an adequate length of time to see the most benefit. Typically, four to six weeks is a reasonable amount of time to use an antidepressant and decide if it is effective for you.
In most cases, the improvement you get from an antidepressant is gradual, and the benefits may be subtle. For example, if tearfulness is a common symptom for you, it might become less frequent. But it is unlikely to disappear right away. If anxiety is a persistent problem, it may slowly diminish and your interest in returning to hobbies and other activities may gradually increase.
Sometimes family members and friends may notice you are doing better before you feel significantly better. With that in mind, try not to rely only on your own perspective. Consider asking the people around you what their impressions are, too.
If you do not see any improvement within four to six weeks, then it may be time for another approach. Your health care provider may recommend you continue taking the same medication, but increase the dose. It is possible that taking another type of medication along with an antidepressant may be helpful. This is called augmentation. The purpose is to use an additional medicine, such as lithium, to boost the effects of the antidepressant.
In addition to medication, adding another type of therapy to your treatment plan may be useful, as well. For example psychotherapy, also known as counseling or talk therapy, often can be effective treatment for depression. Several kinds of psychotherapy are available. Your health care provider can help you decide which one may be right for you.
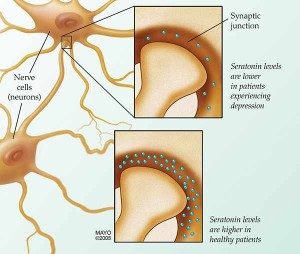
Switching to a different antidepressant is an option, too. Usually a medication from a class of drugs known as selective serotonin reuptake inhibitors, or SSRIs, is the first line of treatment for depression. These include medications such as fluoxetine (Prozac), paroxetine (Paxil) and sertraline (Zoloft).
Other types of antidepressants are available, though, if SSRIs are not effective for you. Among them are drugs known as serotonin and norepinephrine reuptake inhibitors, or SNRIs, and norepinephrine and dopamine reuptake inhibitors, or NDRIs. Studies have shown most antidepressants to be comparable across classes. That means there is no need for you to be on one certain type of antidepressant. You can work with your health care provider to find the one that best fits your needs and circumstances.
Communication with your health care provider is key to developing an effective plan for treating depression. It is important that you feel comfortable talking with him or her about your symptoms and how you are doing. If you do not feel you have good rapport with your provider or if communication is challenging, you may want to consider seeking a second opinion.
Also, keep in mind that if your symptoms get worse at any point, it is critical for you to contact your provider to reassess your situation. The two of you can then decide if you need to make changes to your treatment plan right away. — Michael Reese, M.D., Psychiatry & Psychology, Mayo Clinic, Rochester, Minn.
Related Articles







