-
Researchers Find Cerebrospinal Fluid Boosts Cancer Cell Aggression
Update, March 11, 2021: This post from January 25, 2021 was updated to include foundational work recently published by Frontiers in Oncology.
In cell studies, Mayo researchers and collaborators have uncovered why tumor cells from glioblastoma are more aggressive in one part of the brain than in others. In an article published in Neuro-Oncology, the authors discuss their findings that the genetic expression of cancer cells changed when they grew close to the brain's aquifer of cerebrospinal fluid. This liquid nourishes brain tissue and helps protect it from being jostled. But cancer cells are more aggressive when they develop near the area where this fluid is made and stored in the brain, called the lateral ventricles.
"Tumors in this location kill patients faster than glioblastoma tumors in other areas of the brain," says Hugo Guerrero Cazares, M.D., Ph.D., a cancer researcher at Mayo Clinic and senior author. "Unfortunately, a little over 50% of cases are in this region of the brain."
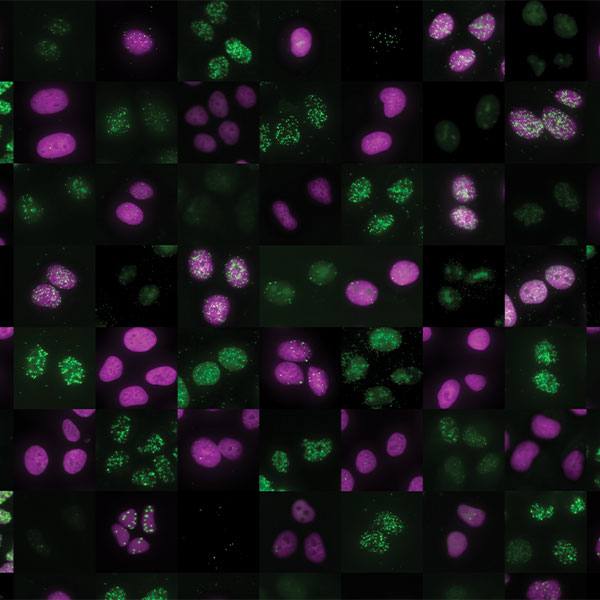
In collaboration with colleagues in Neurologic Surgery, Dr. Guerrero Cazares and his team received brain tumor tissue and cerebrospinal fluid from patients who consented to take part in research. The team anticipated that exposure to cerebrospinal fluid would change the behavior of the cancer cells, and they wanted to know why. Montserrat Lara-Velazquez, M.D., Ph.D., completed the testing for the cell model to validate the hypothesis as part of her doctoral thesis project. From that information, they confirmed that gene expression changed when the cancer cells were in the presence of the fluid. They found that the gene expression changes were stronger when the cerebrospinal fluid came from patients with brain tumors.

"We identified a specific gene that appears to be crucial in this response," says Dr. Guerrero-Cazares. "It indicates that targeting the expression of this gene is a potentially therapeutic approach."
The change was primarily in the gene Serpina3. This gene contains a code for a protein that blocks the action of a type of enzyme. In glioblastoma cells where this gene was blocked, researchers found that the cells had decreased aggression: migration, invasion, proliferation and fewer stem cell characteristics. In a model where the gene was overexpressed, the authors found that glioblastoma cells had increased migration and invasion characteristics.
"This knowledge increases our understanding of the multiple ways the brain microenvironment affects the already aggressive glioblastoma tumors, and in particular, it identifies potential therapeutic targets for this patient population," explains Dr. Guerrero-Cazares.
This finding contributes to diagnostic advancement by providing an additional way to assess patient prognosis. Also, it provides researchers a target for drug development.
"Our next steps are to work to target the expression and activity of this gene," says Dr. Guerrero-Cazares. "Unfortunately, there are no known drugs to target it, so we need to start from scratch in the development of these agents."
Foundational Work
Foundational research on glioblastoma and cerebrospinal fluid, published in Frontiers in Oncology, originally helped Dr. Guerrero-Cazares' lab zero in on this association. Led by Mayo Clinic neuroscientist Anna Carrano, Ph.D. and Dr. Guerrero-Cazares, the study had the team collecting samples right from the operating room, and then whisking them into the lab for more detailed analysis. They mixed the fluid with human brain cancer cell lines and tested the fluid/cell mixture in a mouse model.

"When mixed with cerebrospinal fluid, the cancer cells moved faster and grew faster in both models," says Dr. Carrano. "This could be representative of how glioblastoma progresses and reoccurs in the body."
In tandem with the gene investigation underway in the lab, Dr. Carrano plans to test therapeutic agents against cerebrospinal fluid components.
"If we can block the interaction between a certain component, a protein, in the cerebrospinal fluid, then glioblastoma tumors may be more responsive to standard therapy," she says. " Anything we can do make it better is something to improve patients' survival."