-
What the heck is a nomogram? And other medical research questions answered.

The Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery focuses on the science of best practice. Best practice in health care, that is.
Across the center, researchers work together with the medical practice to find ways to improve health, and the ways people (patients, caregivers, providers) experience health care. This includes identifying what adds value to care experiences, and where we can find cost savings. Health care delivery research encompasses diverse areas, such as human-centered design, data collection and analysis, systems and physical engineering, qualitative research, and much more.
So much research is going on at Mayo Clinic that it’s hard to get our arms around it, and even just within the center, it can be a challenge. But we want to share what we can. We’ve all heard the statistic that it takes 17 years for a practice changing research finding to actually change practice. While that may not always be the case, we figured we’d do our part to spread the news, and maybe shave off a few days here and there.
Here’s a couple of our latest for:
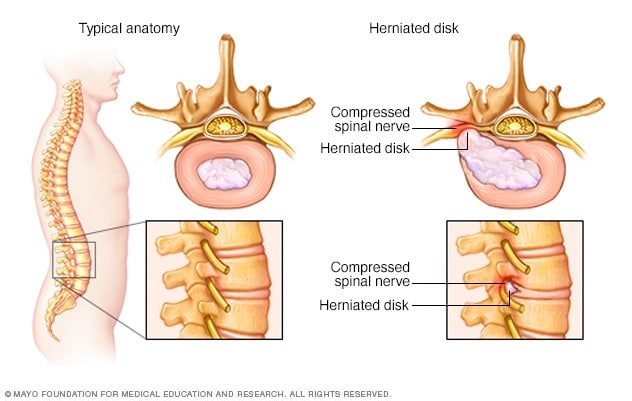
People with herniated disks
Researchers from our Knowledge Synthesis group partnered with others from the Neuro-Informatics Laboratory to dig through all the publications available discussing extraforaminal disk herniation. This particular type of herniation is difficult to diagnose – and treat – because of where it occurs. However, they account for as many as 11 percent of all disk hernias.
The question of how best to treat this condition came from two areas in Mayo Clinic:
- Department of Neurologic Surgery, which provided content expertise about the target condition and type of surgery; and
- Division of Preventive, Occupational and Aerospace Medicine, which provided methodological and analytical expertise.
Together they made up the rest of the research team.
One might assume there would be a commonly understood best practice for how to treat them. But as the research team says in its paper, “Despite the heterogeneity of spinal procedures, there is a paucity of literature comparing the outcomes from different surgical approaches.”
When they completed their search for relevant studies, they found 41 studies with 1,810 patients. Of these, about two-thirds had received open surgery, and the remaining third minimally invasive surgery. Volume does not indicate best practice though.
The team found that compared to open surgery; minimally invasive procedures resulted in lower estimated blood loss, shorter operative times, shorter hospital stays, and faster return-to-work times. They also found that tubular microscopic procedures for extraforaminal disk herniation have the lowest reoperation rate of all minimally invasive surgery types.
Sounds like a cost saving, value adding, experience enhancing finding to me!
Women with breast cancer
is another area we constantly are seeking best (and better) practices. Recently a research team with members from the center and a number of areas across Mayo Clinic including: Surgery, Diagnostic Radiology, Anatomic Pathology, Mayo Clinic School of Medicine, and Health Sciences Research, published a paper describing a new nomogram they developed.
 First you may be wondering, what the heck is a nomogram?
First you may be wondering, what the heck is a nomogram?
Basically it’s a set of lines that each have a scale marked off—in this case lines representing different characteristics of a type of non-invasive breast cancer (ductal carcinoma in situ)—and arranged in a way that connecting a straight line between two known characteristics will allow you to determine a third one.
The team’s nomogram is able to predict which women will actually be found to have invasive breast cancer (a more serious form of the disease) when they go in to have the ductal carcinoma in situ (DCIS) removed.
Doctors can help their patients make more informed decisions before surgery using this new nomogram.
If a woman having a lumpectomy for DCIS is found to have invasive disease, she often will have to come back for a second surgery. However, with this new tool, if the lines predict the woman will have invasive breast cancer, she may wish to have a different surgery up front. She also can go into surgery agreeing to a more aggressive surgery at the time if invasive cancer is seen by the surgeon.
One of the team members we’re especially proud of is Brittany Murphy, M.D. She just completed her time as a Surgical Outcomes Research Fellow in the center, and is well on her way to a great career as a breast surgeon and health care delivery researcher.
The nomogram is likely to be a welcome addition to her and other breast surgeons’ toolkits, and a boon for patients.
About 800 words is all there’s time for today, but check out our website and stay tuned for other updates from the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery.
###
For more research news from Mayo Clinic, you can:
- Subscribe to this blog
- Check out Discovery’s Edge, Mayo’s online research magazine
- Visit the Mayo Clinic Research website
Related Articles