-
Featured News
Mayo Clinic Q and A: Chronic Hives Come and Go With No Clear Pattern

DEAR MAYO CLINIC: I woke up this morning with itchy, red welts covering my arms and legs. These have shown up every now and then over the past few months, and now they seem worse than usual. What could be causing this? How is it treated?
ANSWER: What you may be experiencing is chronic hives. Hives (urticaria) are raised, red or white itchy welts on your skin. A sudden onset of hives (acute hives) usually has an identifiable cause or trigger — such as insect stings or bites, medications, certain foods, allergens, or infections. Acute hives go away within a few weeks and are usually effectively treated with antihistamines.
Chronic hives are different in that they persist for more than six weeks. The hives seem to come and go with no clear pattern — fading over the course of a day or two and then reappearing in a different location a few days later.
Anyone can develop chronic hives, but they’re more common in middle-aged women. Chronic hives can go on for months and even years. They can interfere with sleep, work and other activities. Itching can be severe and may be accompanied by painful swelling. Signs and symptoms tend to flare up with heat, exercise or stress.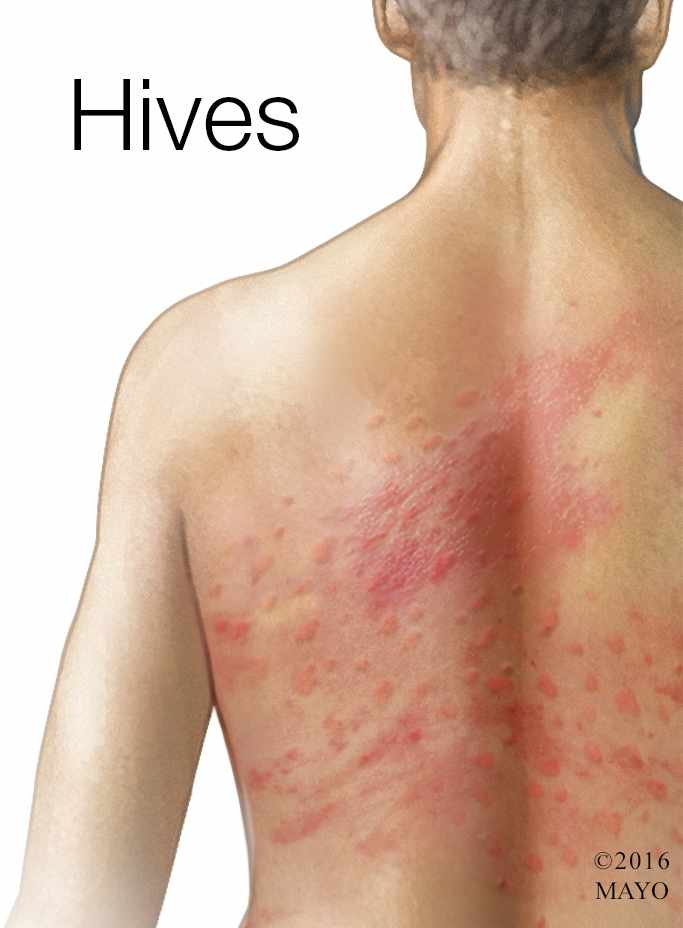
One of the biggest sources of frustration with chronic hives is wondering what’s causing them. The truth is that it’s hard to know. Up to 90 percent of cases remain unexplained — no external factor or contributing disease can be pinpointed as the cause.
People with chronic hives often are anxious that the hives may be a sign of a serious problem. While it’s possible for chronic hives to be associated with an underlying illness, such as an infection, autoimmune disorder or certain cancers, this is pretty rare.
A sudden onset of hives can be part of a serious allergic reaction (anaphylaxis). Signs and symptoms may also include swelling of your tongue or throat, breathing problems, and vomiting. And while anaphylaxis requires emergency care, chronic hives don’t put you at any sudden risk.
To make an accurate diagnosis, your doctor will want to examine your hives. This may mean seeing your doctor when the hives show up. Your doctor also will want to know how often they appear, how long they last, whether you have any painful swelling, and if you have any other signs and symptoms, such as fever, unintentional weight loss, sensitivity to cold or heat, or pain in your abdomen, bones or joints. If your physical exam and medical history suggest there might be an underlying problem causing the hives, your doctor may recommend additional testing, such as blood tests or skin tests.
If the pattern of your symptoms is consistent with chronic hives, your doctor will want to know if you’ve started any new medications, traveled recently, or had any infections or other illnesses that might be contributing to the hives.
Providing your hives aren’t complicated by any additional signs and symptoms, and they can’t be explained by any recent changes in your life, your doctor may recommend starting treatment with an over-the-counter nondrowsy antihistamine every day. Common examples include loratadine (Claritin, Alavert), fexofenadine (Allegra) or cetirizine (Zyrtec). If this doesn’t work for you, be sure to tell your doctor. He or she may increase your dose or try a different kind of antihistamine. Medications such as corticosteroids or histamine (H2) blockers also are possibilities. If antihistamines don’t control the hives, your doctor may prescribe treatment with omalizumab (Xolair), an injectable medicine that’s usually given once a month. In most cases, an effective treatment can be found.
Evidence suggests that certain factors — such as heat, tight clothing and nonsteroidal anti-inflammatory drugs (NSAIDs) — can worsen chronic hives. Try to keep cool, avoid hot showers, and wear loose, comfortable clothing. If you take NSAIDs regularly for pain relief, talk to your doctor about switching to a different form of pain reliever, at least while you continue to have hives.
People often wonder if something in their diets might be causing their hives. There’s very little evidence that certain foods or food additives are responsible for chronic hives. But you may want to keep a food journal alongside a record of your symptoms so that you can detect a pattern, if any. Most doctors don’t recommend any specific diet or dietary elimination.
Although you may never know the cause of your hives, you can rest assured that chronic hives are often temporary. Investigators followed more than 200 people with chronic hives for up to five years. They found that about half the people with unexplained chronic hives were free of symptoms within a year. In the majority of cases, chronic hives can be successfully controlled with medications and possibly a few lifestyle changes. (adapted from Mayo Clinic Health Letter) — Dr. James Li, Allergic Diseases, Rochester, Minn.







