-
Noninvasive test may help some patients with melanoma avoid lymph node biopsy

A Mayo Clinic-led research team has developed a test for patients who have melanoma, the most serious form of skin cancer, that shows whether they're at risk of the cancer spreading to other areas of the body.
The research, described in the journal JCO Precision Oncology, could allow some patients at low risk of metastasis to avoid having a sentinel lymph node biopsy, an invasive surgical procedure that turns out to be negative for 80% of patients.
"The test combines genetic information from a skin biopsy with certain patient characteristics," says Alexander Meves, M.D. , a Mayo Clinic dermatologist and researcher whose laboratory works on cutting-edge methods to diagnose and treat melanoma. "The test tells patients whether their melanoma is so low-risk of spreading to other areas of the body that they do not need to undergo a sentinel lymph node biopsy."
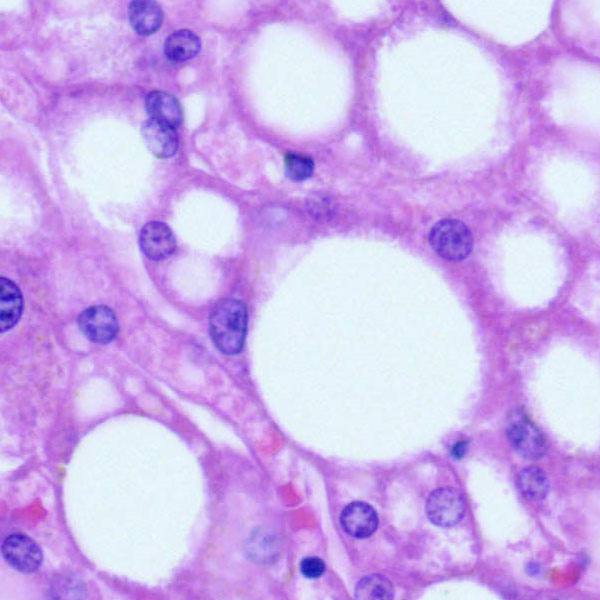
Melanoma develops in the cells that produce melanin, the pigment that gives skin its color. Skin cancer is the most common of all cancers, according to the American Cancer Society. Melanoma accounts for only about 2% of skin cancers but causes a majority of skin cancer deaths, and the rate of incidence has increased markedly in recent years.
The study involved Mayo Clinic researchers in Arizona, Florida and Minnesota, with assistance from a Dutch biotech company, SkylineDx. "We sought to identify molecular tools that indicate which cancer cells are likely to spread throughout the body and determine whether we could identify their presence with a test," says Dr. Meves, the study's senior author. First author is Domenico Bellomo, Ph.D., head of bioinformatics-melanoma at SkylineDx.
The study involved 754 patients who were diagnosed with melanoma at Mayo Clinic campuses in Arizona, Florida and Minnesota between 2004 and 2018. The patients had thin or intermediate thickness primary cutaneous melanoma tumors. The characteristics of the tumors, as well as the patient age at the time of diagnosis, were among the clinical factors taken into account along with gene expression from the tumor.
"This test, which incorporates key clinical and new genomic factors, outperforms all other diagnostics tools in identifying patients with a low risk of nodal metastasis and has the potential to reduce sentinel lymph node biopsy rates by up to 40% while keeping the false omission rate below 5%," says Tina Hieken, M.D., a Mayo Clinic surgical oncologist whose specialty interests include melanoma.
The next step will be to validate the results in a larger prospective study, says Dr. Hieken, a study co-author. "We're working on activating a registry trial to validate these results across key national and international sites," she says.
Previous efforts to identify and validate molecular risk factors have been limited by the small number of patients and incomplete patient data. "We estimate that our test could eliminate as many as 70% of sentinel lymph node procedures for early stage melanoma and 40% of slightly more advanced melanoma, called T2 melanoma," Dr. Meves says.
The study was funded by grants from the National Cancer Institute and the National Center for Advancing Translational Sciences, as well as the Mayo Clinic Center for Individualized Medicine, the Mayo Clinic Cancer Center and the Fifth District Eagles Cancer Telethon.
Dr. Meves reports a financial interest in the test being developed by SkylineDx. Mayo Clinic has reviewed this relationship and taken appropriate steps to protect the scientific integrity of the research.
Learn more
Read more stories about advances in individualized medicine.
Register to get weekly updates from the Mayo Clinic Center for Individualized Medicine blog.
Join the conversation
For more information on the Mayo Clinic Center for Individualized Medicine, visit Facebook, LinkedIn or Twitter at @MayoClinicCIM
Related Articles