-
Individualized Medicine
10 pioneering studies from Mayo Clinic’s Center for Individualized Medicine in 2024
In 2024, collaborative efforts with Mayo Clinic's Center for Individualized Medicine led to significant advances in understanding the biology that shapes health and disease. From new treatments for rare diseases to artificial intelligence-powered tools that help personalize care, these 10 studies exemplify this year’s transformative progress.
1. Innovative tool measures health of a person’s gut microbiome
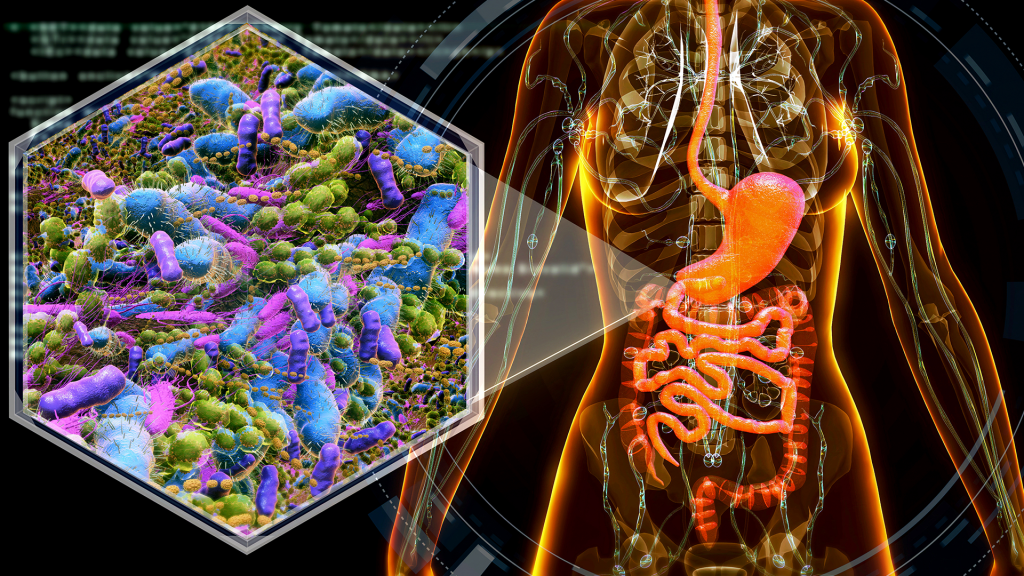
Mayo Clinic researchers, led by Jaeyun Sung, Ph.D., developed an innovative computational tool that analyzes the gut microbiome, a complex ecosystem of trillions of bacteria, fungi, viruses and other microorganisms within the digestive system, to provide insights into overall well-being. In a study published in Nature Communications, the tool demonstrated at least 80% accuracy in differentiating healthy people from those with any disease. The tool, called Gut Microbiome Wellness Index 2, could detect even subtle changes in gut health, identifying whether a person may be progressing toward or recovering from a disease.
"Finally, we have a standardized index to quantitatively measure how healthy a person's gut microbiome is," says Dr. Sung, the senior author and computational biologist at Mayo Clinic Center for Individualized Medicine's Microbiomics Program. Read more.
2. Mayo Clinic’s largest-ever exome study offers blueprint for biomedical breakthroughs

Mayo Clinic's Center for Individualized Medicine reached a significant milestone with its Tapestry study, generating the clinic's largest-ever collection of exome data. This dataset, published in Mayo Clinic Proceedings, focuses on protein-coding genes that play a key role in understanding health and disease. Led by Konstantinos Lazaridis, M.D., the study analyzed DNA from over 100,000 participants from diverse backgrounds, providing important insights into certain genetic predispositions to support personalized and proactive medical guidance. Along with its impact on participants' healthcare, one of the most significant outcomes of the study is the creation of a comprehensive genetic data repository to increase the potential for breakthroughs across different fields of medicine.
"The implications of the Tapestry study are monumental," says Dr. Lazaridis, the Carlson and Nelson Endowed Executive Director for the Center for Individualized Medicine. "As this study continues to inform and transform the practice of personalized medicine, it also sets a new standard for how large-scale medical research can be conducted in an increasingly digital and decentralized world." Read more.
3. Pioneering technology helps solve the unsolvable in rare disease diagnoses
In a significant advancement for rare disease research, Mayo Clinic scientists developed a semi-automated system, known as RENEW, to rapidly reanalyze unresolved rare disease cases. Described in a study published in Human Genetics, RENEW (REanalysis of NEgative Whole-exome/genome data) provided probable diagnoses for 63 of 1,066 undiagnosed cases. This innovative technology, launched in 2022, continuously compares patient genomic data against the latest global research, uncovering previously elusive genetic variants linked to disease.
"Considering that the majority of patients with rare diseases who undergo genomic sequencing remain without a diagnosis, this is no small accomplishment," says Alejandro Ferrer, Ph.D., a translational omics researcher at Mayo Clinic's Center for Individualized Medicine and lead author of the study. "Each successful diagnosis facilitated by RENEW signifies a profound breakthrough in providing answers and hope to people navigating the complexities of rare diseases." Read more.
4. Mayo researchers develop AI-enhanced strategy to personalize medication alerts
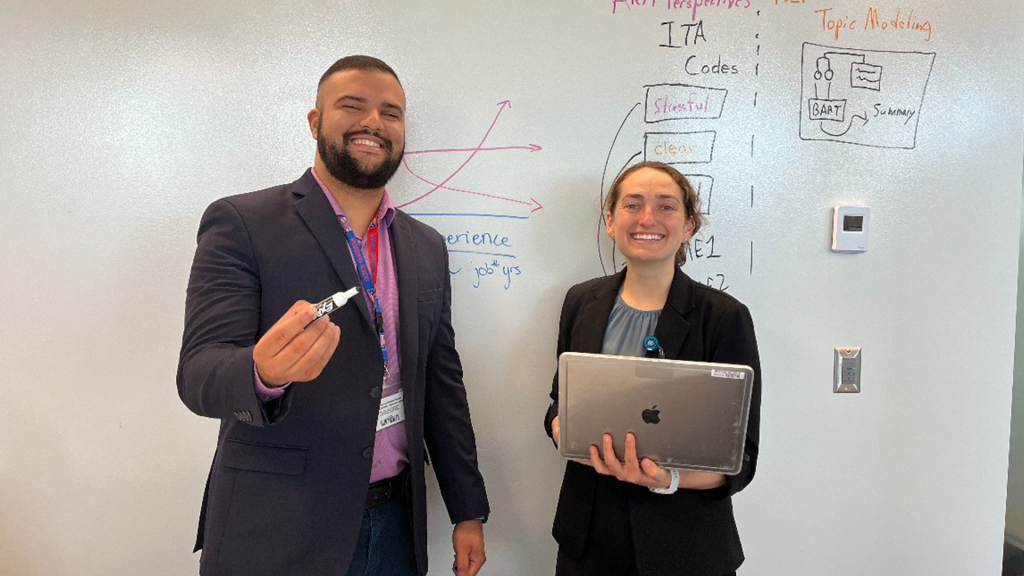
Mayo Clinic researchers have developed an innovative artificial intelligence-enhanced system to deliver medication alerts that are more personalized and actionable. Published in Clinical and Translational Science, the study highlights how the system uses patient-specific genomic data to create concise alerts tailored to individual care needs, moving away from generic, overly detailed notifications. This advancement, led by Arjun Athreya, Ph.D., and his graduate students, represents a step forward in integrating genomic insights into routine care to improve clinical decision-making.
"AI has the potential to greatly enhance how we deliver care by providing vital support with enhanced information to clinicians and researchers, but we need to know the barriers of technology use and factors that may improve human-technology interaction," says Dr. Athreya, a computer scientist at the Mayo Clinic Department of Molecular Pharmacology and Experimental Therapeutics. Read more.
5. Mayo Clinic’s high-tech pursuit of precision alcohol addiction treatment
In an innovative approach to treating alcohol addiction, Ming-Fen Ho, Ph.D., and Richard Weinshilboum, M.D., explored the role of genomics in personalizing therapies. Their study, published in Brain, Behavior and Immunity, revealed genetic variations that influence responses to medications, providing insights into why treatments work for some patients but not others. Their research paves the way for personalized therapy strategies that are precisely tailored to each patient's genomic profile.
"We've discovered that variations in the IL17RB gene can influence treatment outcomes, affecting important factors like how quickly someone might relapse and how long they can stay in recovery," says Dr. Ho, a lead author and a stem cell biologist in the Department of Psychiatry and Psychology. Read more.
6. Genetic cancer risks uncovered in 550 patients
A Mayo Clinic study, published in JCO Precision Oncology, revealed gaps in genetic screening protocols, particularly among underrepresented minorities, for mutations linked to hereditary cancer syndromes. As part of the Tapestry project, researchers sequenced the exomes of over 44,000 participants, identifying 550 carriers of hereditary mutations. Notably, half were unaware of their risk, and 40% didn’t meet clinical testing guidelines.
"This study is a wake-up call, showing us that current national guidelines for genetic screenings are missing too many people at high risk of cancer," says lead author, Niloy Jewel Samadder, M.D., a Mayo Clinic gastroenterologist and cancer geneticist at the Center for Individualized Medicine and the Mayo Clinic Comprehensive Cancer Center. "Early detection of genetic markers for these conditions can lead to proactive screenings and targeted therapies, potentially saving lives of people and their family members." Read more.
7. Innovative blood test may improve mesothelioma detection rate in blood
A team led by Aaron Mansfield , Ph.D., developed a blood test potentially capable of detecting mesothelioma with greater accuracy than current methods. The test identifies complex DNA patterns linked to the disease, enabling earlier diagnosis and treatment for patients with this aggressive cancer. By improving detection rates, the study could significantly impact survival outcomes for mesothelioma, which is often diagnosed in its later stages. The proof-of-concept study was published in the Journal of Thoracic Oncology Clinical and Research Reports.
“We're pushing the frontiers of what's possible in blood-based monitoring," says Dr. Mansfield, a medical oncologist and lead author of the study at the Center for Individualized Medicine and the Mayo Clinic Comprehensive Cancer Center. "Improving detection rates could offer insights into monitoring patients' responses to therapy and detecting recurrence after surgery." Read more.
8. Scientists invent immunotherapy technique to treat autoimmune diseases
Mayo Clinic scientists have developed an immunotherapy strategy that potentially lays the groundwork for treating a spectrum of autoimmune diseases. The new technique, detailed in a preclinical study published in Nature Biomedical Engineering, involves combining chimeric antigen receptors (CAR) with mesenchymal stromal cells (MSC), resulting in engineered stem cells known as CAR-MSCs.
“The pioneering approach shows potential in targeting inflammatory disease sites more precisely and improving immunosuppression and healing outcomes,” says Saad Kenderian, M.B., Ch.B., a principal investigator and hematologist at Mayo Clinic. “We’re planning to study interventions that minimize the need for long-term medications for autoimmune diseases.” Read more.
9. New class of AI may improve cancer research and treatments
Mayo Clinic researchers, led by Hu Li, Ph.D., developed a new class of artificial intelligence to improve cancer research and treatments. By analyzing tumor data at an unprecedented level of detail, this technology enables scientists to identify specific cancer subtypes and tailor therapies to individual patients. The innovation, detailed in Cancers, holds potential for enhancing treatment precision and effectiveness, particularly for aggressive or treatment-resistant cancers.
"This fosters a new era in designing targeted and informed AI algorithms to solve scientific questions, better understand diseases, and guide individualized medicine," says senior author and co-inventor Dr. Li, a Mayo Clinic Systems Biology and AI researcher in the Department of Molecular Pharmacology and Experimental Therapeutics. "It has the potential to uncover insights missed by conventional AI." Read more.
10. Innovative blood analysis technique reveals insights into giant cell arteritis
Mayo Clinic researchers, led by Jaeyun Sung, Ph.D., and Kenneth Warrington, M.D., discovered protein patterns in the blood that could improve the diagnosis and monitoring of giant cell arteritis. This chronic autoimmune disease causes inflammation in blood vessels and can lead to vision loss or stroke if untreated. The study, published in Annals of the Rheumatic Diseases, analyzed over 7,000 proteins using proteomics. Researchers developed machine learning models that identified active disease versus remission with over 95% accuracy. This work lays the foundation for more precise diagnosis and personalized treatment options.
"This precision enables us to refine treatment decisions," says Dr. Warrington, a rheumatologist and Director of the Vasculitis Clinic in the Division of Rheumatology in the Department of Internal Medicine. "Recognizing when a patient's disease is in remission allows us to reduce reliance on certain medications, which can minimize side effects and improve overall patient care." Read more.







