-
3D models of uveal melanoma offer hope for improved treatments
Mayo Clinic researchers have developed organoid models to study uveal melanoma, one of the most common types of eye cancer in adults. Their goal is to use these models to better understand how this disease works and develop treatments for unmet patient needs.
Organoids are 3D models grown from patient tissue that accurately reflect a patient's unique genetic and biological characteristics, also known as "avatars." When derived from a patient's cancer tumor, an organoid will behave and respond to treatments outside the body in a lab (in vitro) just like the original tumor would inside the body (in vivo).
In 50% of patients, uveal melanoma metastasizes, spreading to other parts of the body, leading to a poor prognosis and average survival of less than two years. Unfortunately, current treatments for this condition often have limited effectiveness, leaving patients and their doctors with few options.
"The hope is that these patient-derived organoid models better represent human cancer in the laboratory," says Lauren Dalvin, M.D., a Mayo Clinic Comprehensive Cancer Center ocular oncologist and surgeon-scientist who is one of the lead researchers. "Using these models as a foundation for drug testing will facilitate new treatment discoveries with higher success rates in clinical trials, ultimately translating to improved outcomes for patients with uveal melanoma."
Growing an eye cancer biobank


In the past, the lack of human disease models representing the entire spectrum of uveal melanoma has created a bottleneck, limiting the ability of scientists to identify effective targets for treatment and prevention. Most laboratory studies have drawn from the same set of commercially available cell lines, which are not representative of the disease and often differ in important ways from the original tumors.
To blast through this bottleneck, a study team led by Dr. Dalvin, in collaboration with Martin Fernandez-Zapico, M.D., a cancer biologist with Mayo Clinic Comprehensive Cancer Center, decided to develop a new, uveal melanoma patient-derived organoid biobank. Their goal is to create a research resource representing the real-world variability of this cancer.
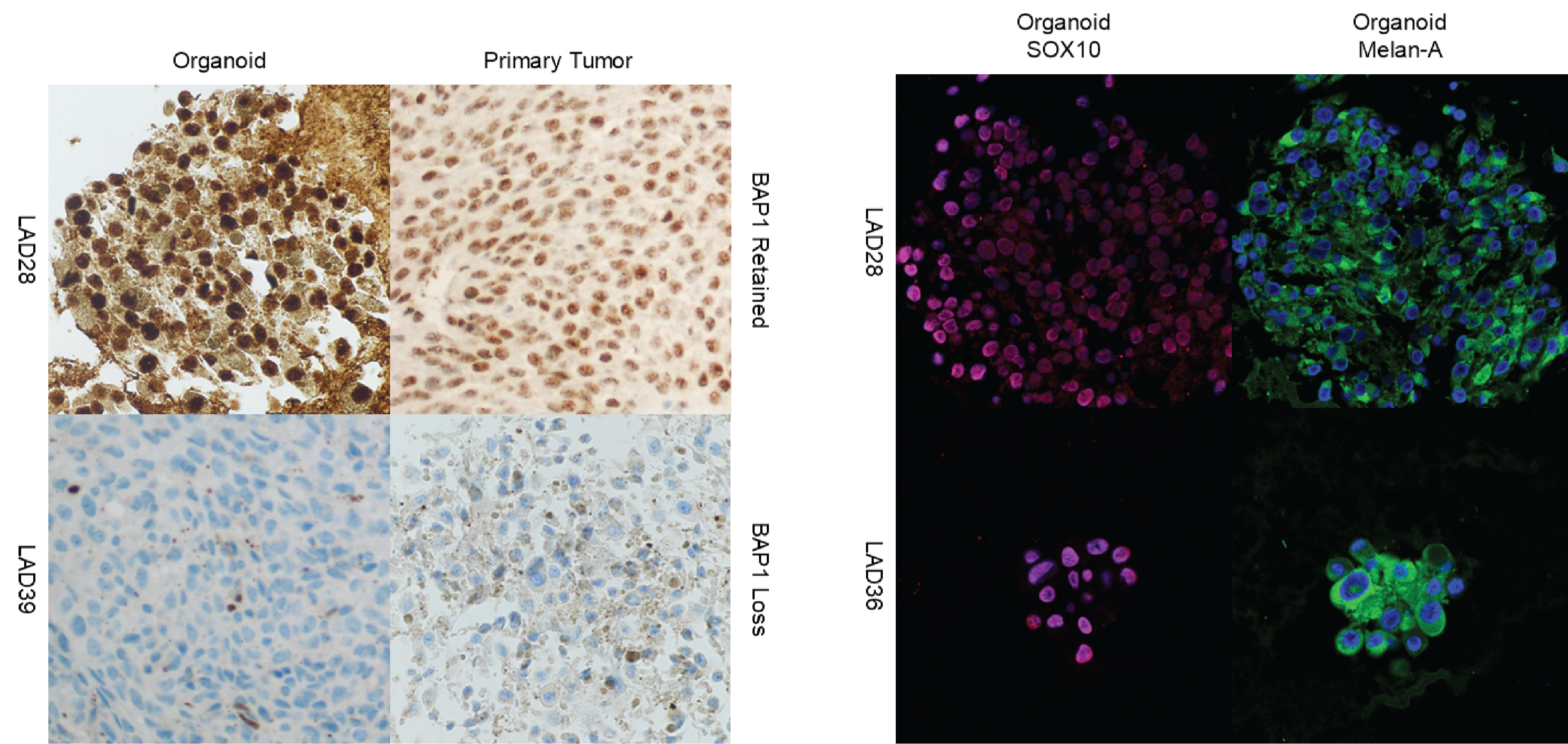
In a paper published in Investigative Ophthalmology & Visual Science, they described the initial development of this biobank. The researchers successfully created organoids derived from Mayo Clinic ocular oncology patients who enrolled in a prospective study involving the collection of tumor tissue for research from July 1, 2019, through July 1, 2024. Their study determined that these organoid models:
- Could be generated, retained their stability through many uses and were a renewable living resource capable of being regenerated at need.
- Retained the clinically relevant features of the original tumors, clustered into appropriate molecular groups based on validated prognostic markers and resembled human disease when compared to in vivo animal models.
- Served as suitable human models for drug screening.
Recognizing the immense value of this organoid biobank, the investigators have already begun expanding it to include other research centers. Their goal is to create a resource capable of representing the global epigenomic variability of uveal melanoma. In the future, they hope this biobank will serve as a comprehensive platform for drug screening and other types of lab research on uveal melanoma. This collaborative effort will accelerate research and pave the way for improved treatments and outcomes for patients with this disease.
Read the paper to learn more about the study, including funding and disclosures.
Mayo Clinic organoid research across the spectrum of disease
Organoids are transforming the landscape of biomedical research. Scientists are using this innovative approach to model diseases, track their progression and identify and characterize potential treatments. Mayo Clinic is at the forefront of organoid research, applying this approach to study a wide range of health conditions including:
- Neurodegenerative and neurological disorders, such as Lewy body dementia, Alzheimer's disease, autism, opioid addiction and alcohol use disorder.
- Measles and other infectious diseases.
- Many types of cancer including breast cancer.
- Inflammatory bowel disease.
The goals of this research extend far beyond its current applications. Mayo Clinic researchers aim to develop organoids representing organs throughout the human body to track disease, screen drugs and regenerate tissues. This approach holds the promise of accelerating research in precision medicine and the search for cures in other areas of biomedical research.