-
Cancer
7 advances in CAR-T cell therapy at Mayo Clinic
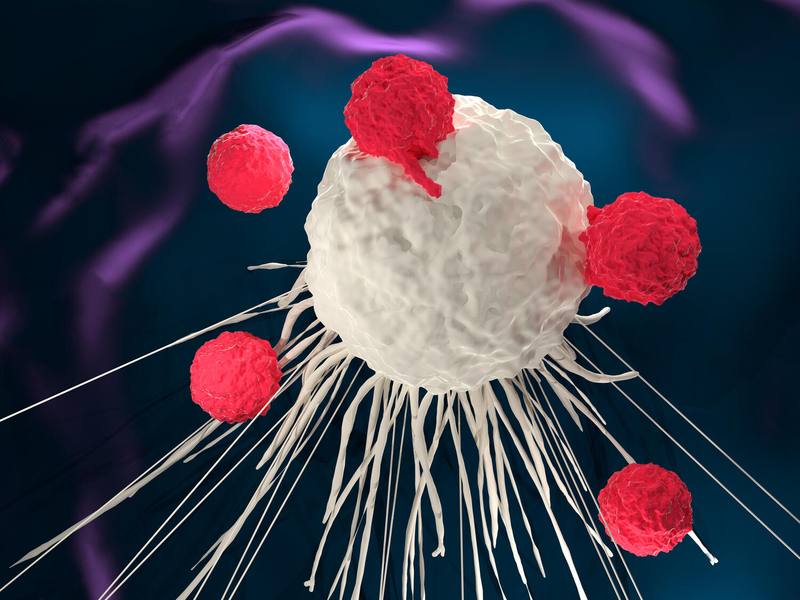
CAR-T cell therapy is a treatment that harnesses the power of a person's immune system to combat cancer cells. In this regenerative immunotherapy, a person's T cells, or white blood cells known as lymphocytes that are involved in the immune system response — are collected and genetically modified to produce chimeric antigen receptors or CARs. They are then infused back into the patient's blood stream, where they target and destroy cancer cells. Mayo Clinic researchers are advancing and improving CAR-T cell therapy to expand its capabilities to treat more conditions. Read more about the latest advances in CAR-T at Mayo Clinic.
CAR-T cell researchers at Mayo Clinic optimistic about future of treating blood cancers
While many CAR-T cell therapies use a patient's own cells, Mayo Clinic is also exploring the applications of allogeneic, or "off-the-shelf," CAR-T therapies. These are generated by healthy donors or gene-edited sources that have been genetically altered to reduce the possibility of rejection by the patient's immune system.
"This can provide a faster turnaround time for manufacturing, expand patient access and allow patients to receive CAR-T cell therapy at the time of need," says Yi Lin, M.D., Ph.D., a hematologist and oncologist at Mayo Clinic Comprehensive Cancer Center.
CAR-T cell therapy is usually offered as a later-stage therapy for various blood cancers, but recent research has shown it may be useful in some blood cancer cases earlier in a patient's treatment plan.
"CAR-T cell therapy in earlier lines of treatment has reported superior outcomes as compared to using it in later lines of therapy," says Rafael Fonseca, M.D., hematologist at Mayo Clinic Comprehensive Cancer Center.
Unleashing CAR-T cell therapy to destroy solid tumors in thyroid cancer
Mayo Clinic researchers are working to apply CAR-T cell therapy to solid tumors in thyroid cancer. CAR-T has shown promising results in blood cancers, and new research is focused on using this treatment on more types of malignancies.
"CAR-T cell therapy is unlike other therapeutics," says Saad Kenderian, M.B., Ch.B., a hematologist and cancer researcher. "Other therapies may slow down cancer. CAR-T cell therapy has shown great promise in stopping B-cell lymphomas and leukemias. Some of my patients have gone into complete remission that has lasted for years after just one treatment."
Could CAR-T cell therapy improve kidney transplants?
CAR-T cell therapy could provide a revolutionary approach to organ transplantation for "sensitized patients" who are hard to match and susceptible to rejection, Mayo Clinic researchers discovered.
Their pioneering research focuses on using CAR-T cells derived from the patient's own immune system to prevent rejection of donated organs. Sensitized patients are those who have high levels of antibodies that cause their immune systems to react negatively to potential donor organs. These patients often face extended waiting periods for a transplant.
Research from this proof-of-concept study is published in Kidney International.
"This research is one of the first steps toward applying CAR-T cells in the field of transplantation to try to make more donor organs available for transplant and reduce the wait for patients who need a new kidney," says Tambi Jarmi, M.D., first author on the study and a transplant nephrologist at Mayo Clinic in Florida.
Mayo Clinic scientists pioneer immunotherapy technique for autoimmune diseases
Mayo Clinic scientists have developed an immunotherapy strategy that potentially lays the groundwork for treating a spectrum of autoimmune diseases.
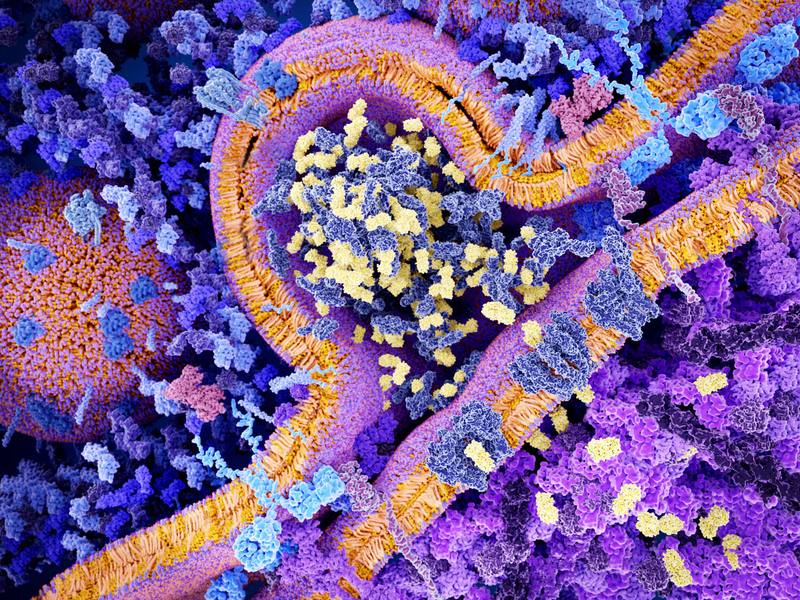
The new technique, detailed in a preclinical study published in Nature Biomedical Engineering, involves combining chimeric antigen receptors (CARs) with mesenchymal stromal cells (MSCs), which are found in various tissues in the body and are known for calming down the immune system, controlling inflammation and promoting immune tolerance to prevent the body's own tissues from being attacked.
"The pioneering approach shows potential in targeting inflammatory disease sites more precisely and improving immunosuppression and healing outcomes," says Dr. Kenderian. "We're planning to study interventions that minimize the need for long-term medications for autoimmune diseases."
Unleashing viruses aimed at killing cancer
Mayo Clinic cancer researcher Richard Vile, Ph.D., is leading research into genetically engineered viruses aimed at unleashing a two-pronged attack on cancer. One part of this technology, known as an oncolytic virus, is designed to infect, break open and destroy cancer cells while sparing healthy tissue. Dr. Vile's preclinical studies have shown that oncolytic viruses replicated in cancer cells and cascaded to kill other diseased cells. That, in turn, triggered an immune response in which the patient's own T cells, stimulated by the virus, recognized and targeted metastasized tumors for a second wave of cancer destruction.
"Oncolytic viruses are a way to alert the immune system and mobilize it to kill cells infected with cancer," says Dr. Vile. "There's the direct killing of cancer cells with the virus, and then there's the major effect of immune activation. The immune system is incredibly well evolved to recognize infection, clear infection and kill all the cells around it that could be harboring infection."
Dr. Vile's team is combining oncolytic viruses with CAR-T cell therapy to target solid tumors from liver cancer. This experimental approach of loading CAR-T cells with oncolytic virus is a new way to expand CAR-T cell therapy beyond treatment for blood cancers into treatment for solid tumors.
Preparing to biomanufacture a new CAR-T cell therapy for B-cell cancers
Mayo Clinic research has developed a new type of CAR-T cell therapy aimed at killing B-cell blood cancers that have returned and are no longer responding to treatment. This pioneering technology, designed and developed in the lab of Hong Qin, M.D., Ph.D., killed B-cell tumors grown in the laboratory and tumors implanted in mouse models. The preclinical findings are published in Cancer Immunology, Immunotherapy.
"This study shows our experimental CAR-T cell therapy targets several blood cancers, specifically chronic lymphocytic leukemia," says Dr. Qin. "Currently there are six different CAR-T cell therapies approved for treatment of relapsed blood cancers. While the results are impressive, not everyone responds to this treatment. Our goal is to provide novel cell therapies shaped to each patient's individual need."
Dr Qin's team developed a cell therapy to target a protein known as B-cell activating factor receptor (BAFF-R) found in patients with B-cell cancers, particularly those with chronic lymphocytic leukemia. The BAFF-R protein is linked to tumor growth. The cell therapy under investigation allows the immune system to quash cancer and target tumors that have returned or have resisted available CAR-T cell therapies.
Using a molecular scissors to improve CAR-T cell therapy
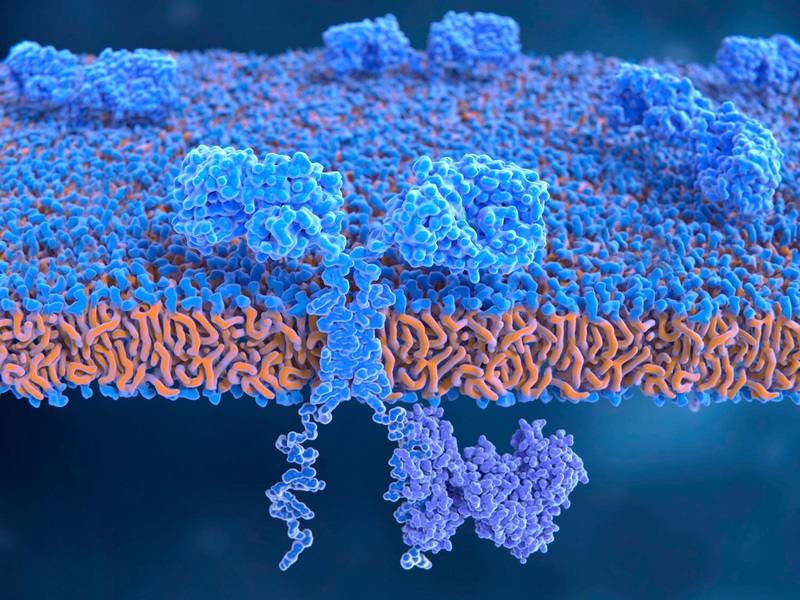
Mayo Clinic researchers who mined the molecular foundations of cancer have uncovered a new reason CAR-T cell therapy fails in some patients. This discovery has fueled new strategies that incorporate antibodies and gene editing to improve the outcome of this breakthrough treatment.
"This is a very exciting discovery that offers new hope of overcoming challenges of CAR-T cell therapy that many cancer patients experience," says Dr. Kenderian, a hematologist and senior author on this research, published in Nature Communications.
"We describe for the first time a mechanism causing the resistance and failure of CAR-T cells, which lies within a protein routinely made by the engineered cells. This research puts us on a new path for improving the longevity of CAR-T cell therapy."