-
Featured News
Asthma medications: Know your options
Confused about your asthma medications? Here's what you need to know to sort out the main classes and numerous subtypes of asthma drugs.
The types and doses of asthma medications you need depend on your age, your symptoms, the severity of your asthma and medication side effects.
Because your asthma can change over time, work closely with your health care provided to track your symptoms and adjust your asthma medications, if needed.
Types of asthma medications
| Category | Purpose | Types |
|---|---|---|
| Long-term asthma control medications | Taken regularly to control chronic symptoms and prevent asthma attacks — the most important type of treatment for most people with asthma |
|
| Quick-relief medications (rescue medications) | Taken as needed for rapid, short-term relief of symptoms — used to prevent or treat an asthma attack |
|
| Medications for allergy-induced asthma | Taken regularly or as needed to reduce your body's sensitivity to a particular allergy-causing substance (allergen) |
|
| Biologics | Taken with control medications to stop underlying biological responses causing inflammation in the lungs — used to better manage severe asthma symptoms |
|
Long-term control medications
Many people with asthma need to take long-term control medications daily, even when they don't have symptoms. There are several types of long-term control medications, including the following.
Inhaled corticosteroids
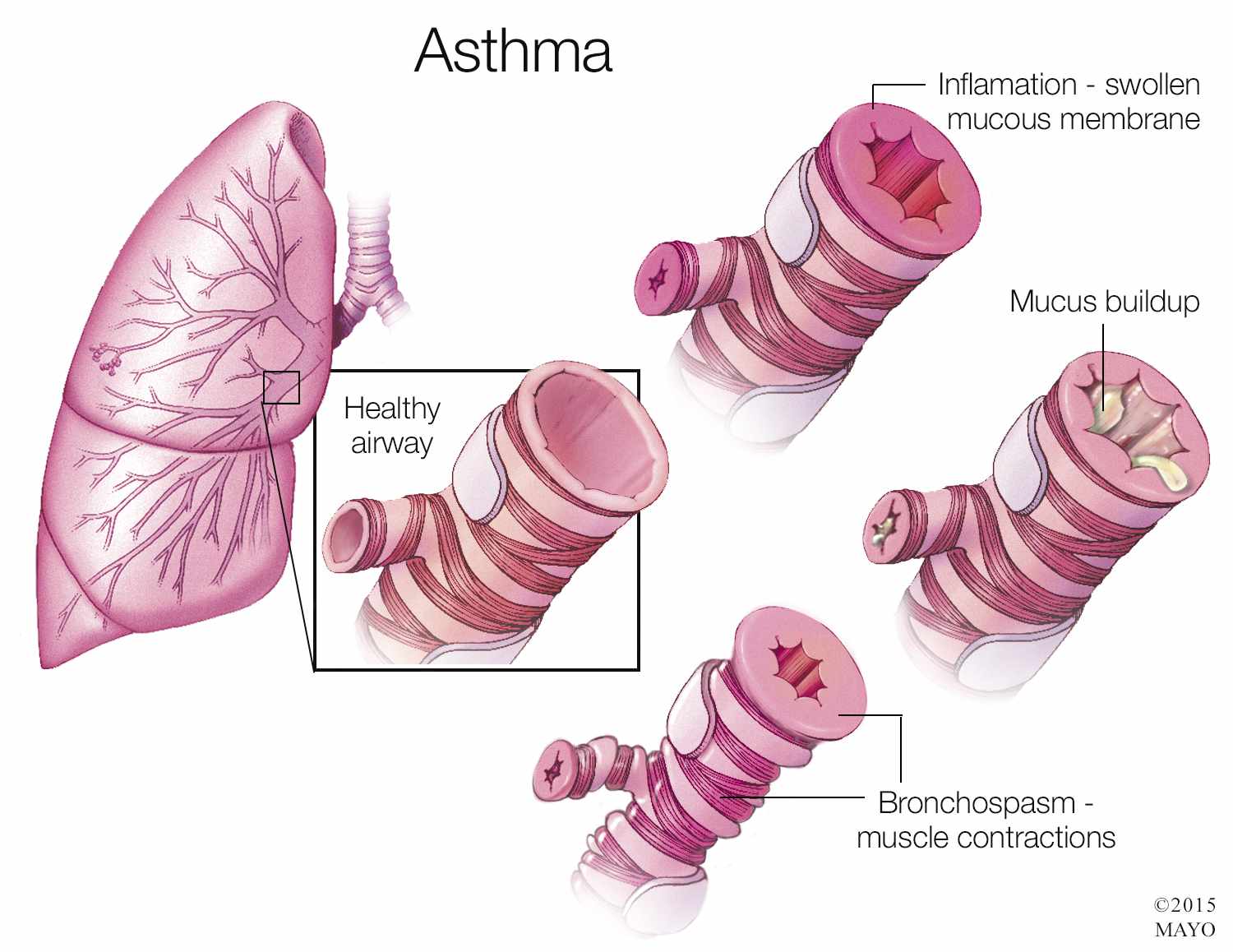
These anti-inflammatory drugs are the most effective and commonly used long-term control medications for asthma. They reduce swelling and tightening in your airways. You may need to use these medications for several months before you get their maximum benefit.
Inhaled corticosteroids include:
- Fluticasone (Flovent HFA)
- Budesonide (Pulmicort Flexhaler)
- Mometasone (Asmanex Twisthaler)
- Beclomethasone (Qvar RediHaler)
- Ciclesonide (Alvesco)
In children, long-term use of inhaled corticosteroids can delay growth slightly, but the benefits of using these medications to maintain good asthma control generally outweigh the risks. Regular use of inhaled corticosteroids helps keep asthma attacks and other problems linked to poorly controlled asthma in check.
Inhaled corticosteroids don't generally cause serious side effects. When side effects occur, they can include mouth and throat irritation and oral yeast infections. If you're using a metered dose inhaler, use a spacer and rinse your mouth with water after each use to reduce the amount of drug remaining in your mouth.
Leukotriene modifiers
These medications block the effects of leukotrienes, immune system chemicals that cause asthma symptoms. Leukotriene modifiers can help prevent symptoms for up to 24 hours. Examples include:
- Montelukast (Singulair)
- Zafirlukast (Accolate)
- Zileuton (Zyflo)
In rare cases, montelukast is linked to psychological reactions, such as agitation, aggression, hallucinations, depression and suicidal thinking. See your doctor right away if you have any unusual reactions.
Long-acting beta agonists (LABAs)
These bronchodilator (brong-koh-DIE-lay-tur) medications open airways and reduce swelling for at least 12 hours. They're used on a regular schedule to control moderate to severe asthma and to prevent nighttime symptoms. Although they're effective, they've been linked to severe asthma attacks. For this reason, LABAs are taken only in combination with an inhaled corticosteroid.
The most commonly used LABA for asthma is salmeterol (Serevent).
Theophylline
You take this bronchodilator daily in pill form to treat mild asthma. Theophylline (Theo-24, others) relaxes the airways and decreases the lungs' response to irritants. It can be helpful for nighttime asthma symptoms. You might need regular blood tests to make sure you're getting the correct dose. Potential side effects of theophylline include insomnia and gastroesophageal reflux.
Combination inhalers: Corticosteroids and long-acting beta agonists
Some inhaled asthma medication combinations contain both a corticosteroid and a bronchodilator:
- Fluticasone and salmeterol (Advair Diskus)
- Budesonide and formoterol (Symbicort)
- Mometasone and formoterol (Dulera)
- Fluticasone and vilanterol (Breo)
Quick-relief medications
These asthma medications open the lungs by relaxing airway muscles. Often called rescue medications, they can ease worsening symptoms or stop an asthma attack in progress. They begin working within minutes and are effective for four to six hours. They're not for daily use.
Some people use a quick-relief inhaler before exercise to help prevent shortness of breath and other asthma symptoms. Possible side effects include jitteriness and palpitations.
Quick-relief medications include:
- Albuterol (ProAir HFA, Ventolin HFA, others)
- Levalbuterol (Xopenex HFA)
If your symptoms are minor and infrequent or if you have exercise-induced asthma, you might manage your symptoms with one of these medications alone. However, most people with persistent asthma also need an inhaled corticosteroid or other long-term control medication.
If you need to use your inhaler more often than your doctor recommends, your asthma is not under control — and you may be increasing your risk of a serious asthma attack.
Ipratropium
Ipratropium (Atrovent HFA) is a short-acting bronchodilator that's usually prescribed for emphysema or chronic bronchitis, but is sometimes used to treat asthma attacks. It may be used either with or as an alternative to short-acting beta agonists.
Oral corticosteroids for serious asthma attacks
These medications may be taken to treat severe asthma attacks. They can cause bothersome short-term side effects and more-serious side effects if they're taken for a long period. Examples include:
- Prednisone
- Methylprednisolone
Long-term use of these medications can cause side effects including cataracts, thinning bones (osteoporosis), muscle weakness, decreased resistance to infection, high blood pressure and reduced growth in children.
Click here to learn more about asthma medications.
This article is written by Mayo Clinic staff. Find more health and medical information on mayoclinic.org.







