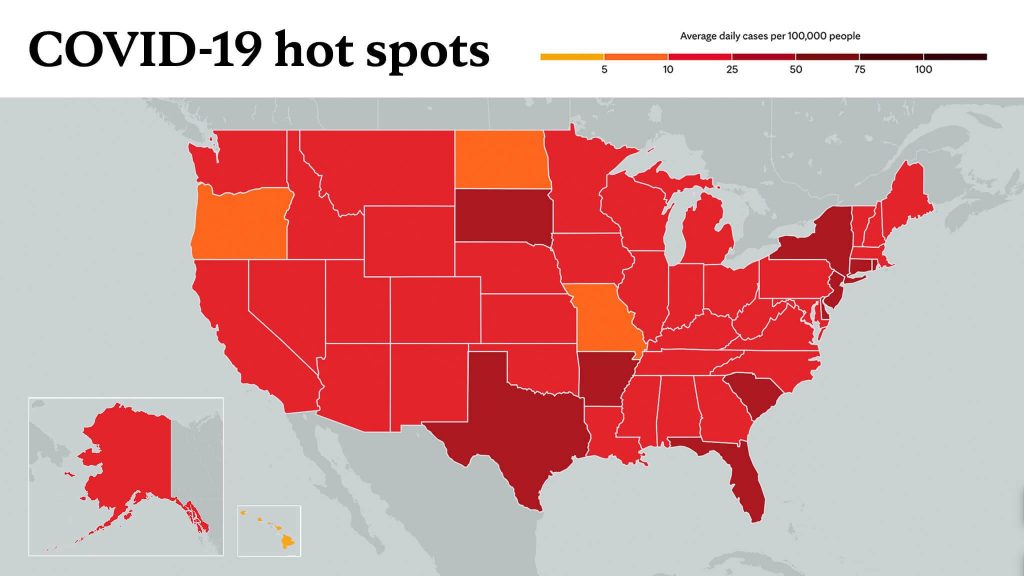
U.S. public health officials report that the COVID-19 pandemic has disproportionately affected communities that have been medically underserved, leading to higher infection and mortality rates. A Mayo Clinic study recently published in the American Journal of Public Health says easy access to rapid testing is needed to combat disparities, and a community-driven and culturally tailored strategy is key for success.
Researchers describe the process of setting up a drive-thru COVID-19 test collection site at Open Cities Health Center, a nonprofit community health center in St. Paul, Minnesota, that primarily provides services to patients with lower incomes, or who are uninsured or underinsured. This effort was collaboratively designed and implemented by Mayo Clinic, the FAITH (Fostering African American Improvement in Total Health) program and community partners at Open Cities Health Center.
During the collaboration period reported in the study, Open Cities Health Center observed an increased demand for testing and a downward trend in COVID-19 positivity rates — indicators of the value of the service. These results garnered recognition and funding from state, national and institutional sources to maintain and expand the testing effort.
FAITH is a community-based participatory research program focused on improving health and wellness within Black communities in Minnesota. The program is led by LaPrincess Brewer, M.D., a cardiologist and health disparities researcher at Mayo Clinic. The FAITH program routinely works with Open Cities Health Center, which provides culturally tailored primary care to more than 10,000 patients who are racially and ethnically diverse, and nearly 50% of whom are Black.
The research team led by Dr. Brewer, first author of the study, adapted Mayo Clinic's existing model of drive-thru COVID-19 nasal swab collections to meet the requirements of Open Cities Health Center and its patients. The team decided to locate the testing site near a public bus line and established a special walk-in policy and procedure to triage people who arrived for testing without an appointment.
"We wanted to serve the community and ensure that everyone had the opportunity to be tested," says Clarence Jones, a leader in the FAITH program and a member of the Open Cities Community Advisory Board. "We created a process to ensure walk-ins could still complete screening as well as testing on the same day."
The team adjusted testing center workflows to accommodate a surge in demand following the death of George Floyd in May 2020, as many community members attended protests and memorial services. They also extended testing eligibility to include recent attendance at mass gatherings, regardless of the presence of symptoms.
The team also disseminated culturally tailored COVID-19 health messaging for Open Cities Health Center's patient population. These messages were included in materials distributed at the testing site, shared with patients via mail and text, and communicated broadly via social media and on the Open Cities Health Center website.
"It was important for community members to receive consistent, culturally appropriate messages in a variety of channels, and to receive this information from people they trust at their community health center and the FAITH program," says Dr. Brewer.
Researchers consider the outcomes of this testing initiative as a testament to the importance of community-academic partnerships.
"This productive collaboration should serve as a model for current and future efforts aiming to improve health equity for all populations," says Cynthia Woods, M.D., interim CEO and medical director, Open Cities Health Center.
The researchers hope this community-based approach can be replicated for future vaccine distribution needs, and that it can help plan and implement interventions to meet emergency health needs in communities that are underserved.
Chyke Doubeni, M.B.B.S., director of the Mayo Clinic Center for Health Equity and Community Engagement Research, is the study's senior author. In addition, a team of Mayo Clinic staff members, FAITH program community partners, and Open Cities Health Center staff also were involved in the study.
This research was supported by Clinical and Translational Science Award grant No. UL1 TR000135 from the National Center for Advancing Translational Sciences to Mayo Clinic, Mayo Clinic's Center for Health Equity and Community Engagement in Research, National Institutes of Health's National Institute on Minority Health and Disparities, and the Centers for Disease Control and Prevention.
Media contact:
- Caitlin Doran, Mayo Clinic Public Affairs, newsbureau@mayo.edu
_______________________________________
Information in this post was accurate at the time of its posting. Due to the fluid nature of the COVID-19 pandemic, scientific understanding, along with guidelines and recommendations, may have changed since the original publication date.
For more information and all your COVID-19 coverage, go to the Mayo Clinic News Network and mayoclinic.org.
Learn more about tracking COVID-19 and COVID-19 trends.