-
Cancer
Detecting pancreatic cancer through changes in body composition and metabolism
Pancreatic cancer is a formidable disease, often diagnosed too late for effective treatment. However, new research from Mayo Clinic represents a promising step toward identifying biological signals or biomarkers that may aid in early detection.
By tracking changes in body composition and metabolism, researchers are working to identify high-risk patients who could benefit from selective screening for the disease, which kills more than 50,000 Americans a year.

"When most patients come to us with pancreatic cancer, their cancer has already spread and their survival over a five-year period is only three percent. But if we catch them early, at stage 1A, their five-year survival rate can be as high as 80%," says Yan Bi, M.D., Ph.D., a gastroenterologist at Mayo Clinic in Florida. "Detecting the cancer earlier is the best way to improve survival."
Early detection is tricky because the first symptoms of pancreatic cancer — digestive issues, belly pain and weight loss — are not specific. "Weight loss occurs even before the diagnosis," says Dr. Bi. "A majority of pancreatic cancer patients will lose weight before they discover they have cancer."
Studies have shown that as the disease progresses, cancer cells promote a wide range of metabolic and physiologic changes. Dr. Bi and her colleagues wondered if these changes could serve as biomarkers, to enable healthcare providers to detect pancreatic cancer earlier than ever before.
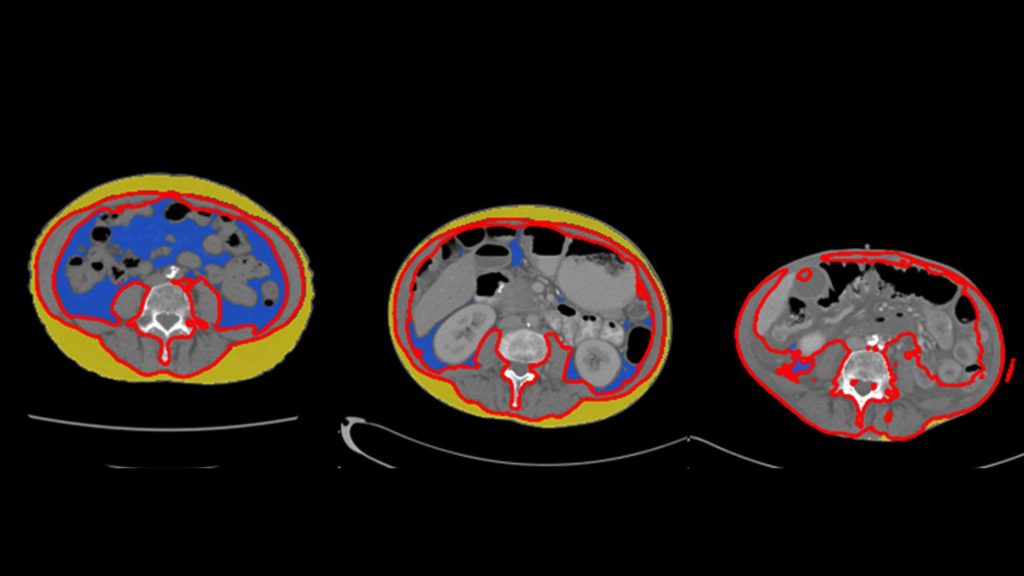
Dr. Bi teamed up with Derk Klatte, M.D., Ph.D., and Michael Wallace, M.D., to examine medical records of patients with a common type of pancreatic cancer known as pancreatic ductal adenocarcinoma (PDAC) who had been diagnosed at Mayo Clinic between 2002 and 2021. They analyzed abdominal CT scans and blood tests taken up to three years before the patients were diagnosed. Using advanced algorithms developed by data scientist Alex Weston, Ph.D., the researchers measured changes in body fat, muscle and bone, as well as shifts in blood-based biomarkers like cholesterol and glucose levels.
The findings, published in the journal Clinical Gastroenterology and Hepatology, revealed changes in a variety of physiological and metabolic measurements. The researchers observed significant reductions in both fat surrounding the organs (visceral fat) and the fat under the skin (subcutaneous fat) as patients approached their diagnosis date. In addition, patients exhibited a notable drop in serum lipids — fats found in the blood — such as low-density lipoprotein (LDL), total cholesterol and triglycerides.
Conversely, the study found that blood glucose levels increased up to three years before patients were diagnosed with pancreatic cancer, confirming a link previously described by Mayo Clinic gastroenterologist Suresh Chari, M.D. Additional findings revealed that patients also experienced a loss of muscle mass and bone volume, which became more pronounced in the last six months before their cancer was detected.
"It is a bizarre condition," says Dr. Bi. "Patients' bodies are changing — they are losing weight and their total cholesterol levels are going down…many things you think would be healthy, but in this case, they're not. Nobody knows exactly what is going on, but we aim to find out."
Dr. Bi recently received two grants, one from the National Institutes of Health and another from the Department of Defense, to investigate how the growth of pancreatic tumors could drive such widespread metabolic changes.
She is also expanding her work on pancreatic cancer biomarkers, searching for the best combination of factors to make an early diagnosis. "We are using many different layers of information — medical records, labs and data gathered from wearable devices," she says.
Dr. Bi is part of the Kern Health Care Delivery Scholars Program in the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. The program supports the next generation of clinically trained, doctoral-level fellows and junior faculty in health services research.
As a Kern Health Care Delivery Scholar, Dr. Bi has been working on a project that uses wearables like Apple Watches or Fitbits to track changes in body composition as well as the power of artificial intelligence (AI).
"My goal is to combine that information with all the other data we have on a patient and use AI to calculate their risk of developing pancreatic cancer in three years," she says. "If they are at increased risk, we could start doing surveillance with abdominal imaging."
The team's early findings suggest that capturing the subtle yet significant body changes that occur as pancreatic cancer develops could be a key strategy in the fight against the disease. Recognizing these changes early could lead to timely diagnosis and treatment, potentially saving lives.
Dr. Bi and her colleagues at Mayo Clinic are active in the Pancreatic Cancer Early Detection (PRECEDE) consortium, a global effort to improve early detection and prevention of pancreatic cancer. The consortium's goal is to increase the five-year survival rate to 50% after 10 years.
"It is very ambitious," she says, "but I hope we can reach that goal by pushing for early detection."
Review the study for a complete list of authors, disclosures and funding.
About Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery
The Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery collaborates with clinical areas across Mayo to create and evaluate data-driven solutions to transform the experience of health and healthcare for patients, staff, and communities. It drives continuous improvement of Mayo Clinic as a learning health system, enabling always safe, evidence-based, high-quality care.







