-
Biotherapeutics
‘Disease in a dish’ research to advance regenerative solutions for MS
A desire to stop the debilitating, life-changing symptoms of multiple sclerosis (MS) inspires Charles Howe, Ph.D., to take his investigation beyond standard research in the quest for regenerative therapies that protect nerves and promote healing. Dr. Howe's team at Mayo Clinic seeks to answer whether axons — the neuronal wires that send brain signals to muscles — might hold a key to unlocking the mystery of how MS progresses. Dr. Howe and his team seek to understand the scientific question of whether there is a regenerative therapy to reverse neuronal damage.
Regenerative medicine seeks to repair, replace or restore damaged tissues, cells or organs to restore form and function. Mayo Clinic's Center for Regenerative Medicine is a driver of this new era of health care that shifts the focus from treating disease to rebuilding health. As such, it supports research to advance regenerative therapies for MS and other diseases of the central nervous system.
"The new holy grail for trying to prevent or cure MS is to understand what we call disease progression," says Dr. Howe. "That is the starting point of finding a cure. More research is needed, because the strategies we're currently using to manage the symptoms are not sufficient to stop the devastating effects of the disease."
A relapsing disease with no cure
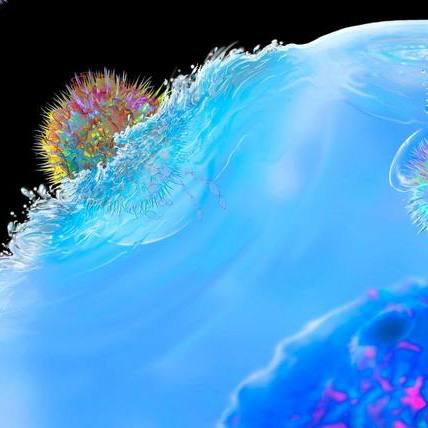
Approximately 1 million people in the U.S. are living with MS, according to the Multiple Sclerosis Association of America. MS is a disease in which the body's immune system attacks the central nervous system, damaging the protective coating on nerves known as myelin. Myelin damage slows or stops nerves from transporting messages between the brain and muscles, resulting in loss of function in speech, vision and mobility.
In most people, MS begins as a relapsing disease. Patients have bouts of symptoms followed by recovery. However, with each incident, the disease progressively worsens until about age 45 when bodily function begins to steadily decline.
"To date, the focus of MS research has been on the cause of myelin loss, or demyelination of the nervous system, and the biological changes in the brain that trigger it. Medication for limiting the relapses has been helpful for slowing disease progression for a period of time, but it isn't a cure," says Dr. Howe. "Eventually almost all patients experience a progressive debilitating loss of function."
Mayo Clinic research investigates additional factors that may contribute to myelin damage, such as age, lifestyle, metabolism and environment. Dr. Howe's Translational Neuroimmunology Lab is zeroing in on the injury of axons and the death of neurons, and whether that can be stopped to halt disease progression.
"Our theory is that demyelination is only one component of MS disease progression. We are focused on the idea that demyelination causes or facilitates the death and destruction of axons, which leads to the accumulation of this progressive loss of function," says Dr. Howe.
A regenerative approach to understanding progression
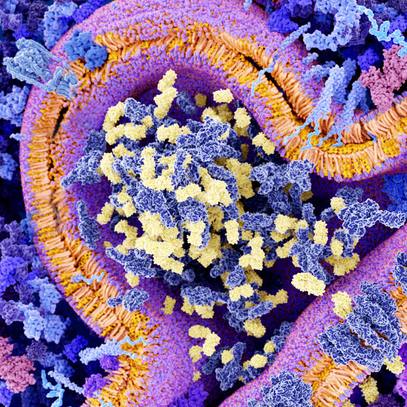
To better understand the role of axons in MS, Dr. Howe's lab is turning to the most humanlike research models possible. His team works with the Regenerative Medicine Biotrust and the Center for Multiple Sclerosis in Autoimmune Neurology to replicate MS as a "disease in a dish." The biotrust collects and stores skin cell fibroblasts from MS patients and then converts them to induced pluripotent stem cells. Induced pluripotent stem cells are adult cells that are reprogrammed to go back in time to a state when they could differentiate into any type of cell or tissue in the body. These cells can be redirected to become neuronal cells that are grown into a 3D model of brain cells with MS. Dr. Howe's team then follows the patient over time to better understand disease progression.
"Dr. Howe's innovative research helps bridge the gap from animal models to human disease by investigating stem cells derived directly from MS patients in order to model injury to the axon, a known driver of irreversible disability in MS. His work has the potential to identify novel therapeutic targets that limit axonal injury in MS, with the hope of preventing or slowing disease progression," says Claudia Lucchinetti, M.D., chair of Mayo Clinic's Department of Neurology, and director of Mayo Clinic's Center for Clinical andTranslational Science and dean of Clinical and Translational Research. Dr. Lucchinetti is the Eugene and Marcia Applebaum Professor of Neuroscience.
A different aspect of Dr. Howe's research focuses on ways to regenerate oligodendrocyte progenitor cells ― cells that provide a protective coating for nerves ― that enable instructional messages to travel throughout the body. Over time, oligodendrocyte progenitor cells become depleted in people with MS.
"Our research is investigating whether there are strategies that would repair the protective myelin coating on nerves by transplanting oligodendrocyte progenitor cells derived from each patient's own skin fibroblast cells," says Dr. Howe. "Evidence in preclinical models has shown this may be effective in reversing the myelin damage that causes loss of function."
Dr. Howe and clinical collaborators also are investigating whether mesenchymal stem cells — adult stem cells that have been well-studied — also might have a therapeutic effect in preventing immune system attacks on nerves.
However, more research is needed to better understand exact causes of disease progression before scientists are ready to test new therapies to repair or replace damage nerves.
"Our ultimate goal is not to suppress the immune system, which is what many of the drugs that are used today for MS do. We'd rather have a drug that targets very specifically the aspect of the immune system that is damaging these axons," says Dr. Howe.
While the goal of finding a new therapy may be years away, Dr. Howe has turned to a more immediate need. His team is working to speed the manipulation of skin fibroblast cells directly into neurons and neural stem cells so that the research can be done in weeks or days rather than months. Making the process more efficient and timelier may increase the likelihood that one day stem cells could be used in a clinical setting to improve care for MS patients.
###