-
Editorial: Why DNA sequencing is an effective tool for patient care
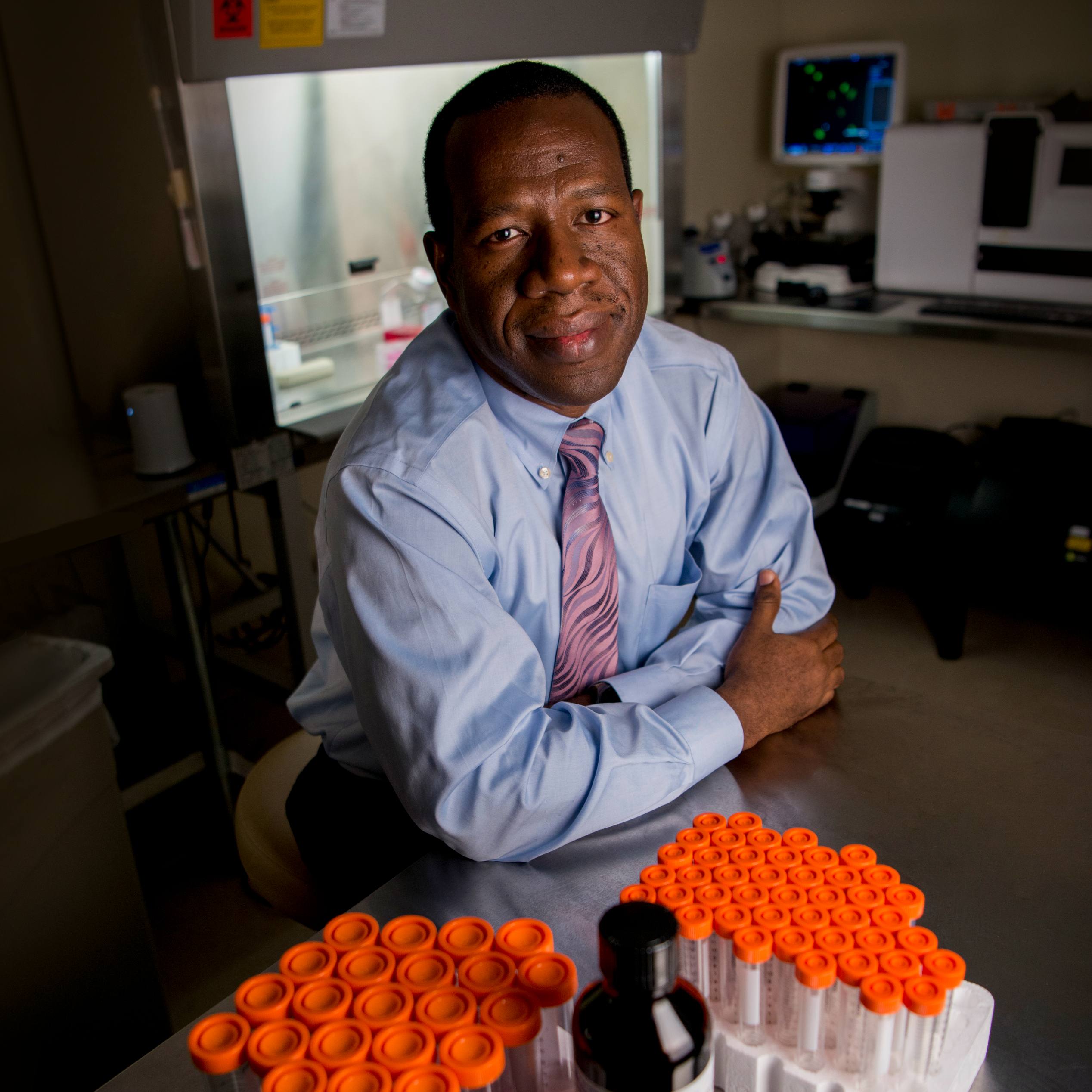
By Keith Stewart, M.B., CH.B.
For the past 30 years, I’ve been fortunate enough to work with and help many patients. But over that time, I’ve also met people who did not respond to therapy or had significant side effects, while others had marvelous responses. Cases like these show a clear need for personalized medicine. Fortunately, I’ve also seen the adoption of a new technology that allows us to gain unprecedented insight into a patient’s specific needs: DNA sequencing.

Everyone has their own unique sequence of DNA — a molecular fingerprint — that determines personal characteristics like height, hair and eye color, and risk for disease. Research has shown us that insights into a person’s DNA sequence allows us to personalize their health care to their own genetic makeup to better meet their needs.*
In the past decade, we’ve seen exponential growth in DNA sequencing technology and an expansion of its use in medicine.* In 2012, Mayo Clinic adopted DNA sequencing as a major tool in individualized medicine by using targeted gene panels and whole exome sequencing. We started by looking for actionable targets in patients with advanced cancers (unique features of a tumor that can make one therapeutic drug particularly effective). We quickly expanded this approach beyond cancer by opening clinics that helped to diagnose rare and undiagnosed diseases.
Rare and undiagnosed diseases
Our patients come from around the world, often seeking a diagnosis for a rare disease that no other doctor or clinic has been able to provide. Whole exome testing sequences more than 20,000 genes. That represents about one percent of a patient’s DNA — the part that we today understand contains the majority of useful genetic information that can pinpoint an illness. Patients can get their DNA mapped and have results within a few weeks to apply to their treatment plans. Prenatal screening could be made less invasive and more comfortable for patients with DNA sequencing, so we did that too. What we found was that DNA sequencing greatly expanded our ability to help patients by providing them with more informed and often more effective health care.
Treatment of cancers
One area where we’ve found DNA sequencing to be particularly effective is in the treatment of cancers.* One example that comes to mind is that of a young girl who had acute lymphoblastic leukemia, an aggressive form of blood cancer. None of the mainline therapeutic strategies had worked for this patient. But thankfully, DNA sequencing identified mutations in the cancer that could be leveraged. It’s clear from this example — and from many more like it — that DNA sequencing is a valuable tool in designing personalized treatments for some cancer patients. But there’s also benefit in potentially preventing the development of cancer in the first place. It’s estimated that between 10-15% of cancers involve a heritable mutation.* Current screening methods used to identify people who are at risk of developing cancer may miss up to 50% of heritable cancers. That leaves a lot of room for improvement, and DNA sequencing is proving to be a valuable tool in this regard.
Prevention of adverse drug reactions
Another valuable application is in the prevention of adverse drug reactions. It’s probably no surprise to learn that some people respond to medicine differently compared to others. In some of these cases, people may even have an unwanted or dangerous response to the drug. These are known as adverse drug reactions, and it’s estimated that approximately 1.5 million of them happen each year in the U.S., resulting in a thousand deaths annually. Research has shown us that some people are genetically predisposed to experiencing an adverse drug reaction, which means there’s an opportunity for DNA sequencing to help identify those individuals and help guide their treatment away from unnecessary risks.
My personal experience
It so happens that I’m one of those individuals. Through DNA sequencing, I found that I should avoid a number of medicines. Most of them are drugs that I will probably never need, but some of them I might. Thanks to this testing, I know what those are and can act accordingly in the future. This brings me to a benefit of DNA sequencing that I think we often overlook. I had my DNA sequenced and got information about my carrier status, potential drug reactions, and a number of health conditions. This was important to me because I have family members whose lives have been affected by a heritable genetic condition. I’ve found that having my DNA sequenced empowers me with knowledge — knowledge that I can use in the future to help guide medical treatment away from potentially dangerous drugs, and maybe even help my health care providers save valuable time if they’re ever looking for a diagnosis. So it’s not just a result that helps me stay informed today; it’s something I will likely use for the rest of my life. To be sure, DNA sequencing is not without its limitations.* When we first started in 2012, we were limited by the cost of sequencing and the time it took to receive and interpret a patient’s results. There is still so much we don’t know about genetics, and research is ongoing to determine how DNA sequencing is best applied. But this research has unlocked new avenues for improving outcomes in recent years, and I strongly believe this trend will continue. In the midst of this DNA sequencing revolution, I’ve had the unique opportunity to explore the field as a researcher, a physician, and an administrator, and I can tell you what an exciting time this is to be learning more about your genetics. My experience has shown me that DNA sequencing is not just a thing of the future — it’s a very real and impactful tool of the present.
Keith Stewart, M.B., CH.B., is the Carlson and Nelson Endowed Director of the Mayo Clinic Center for Individualized Medicine.
1. Manolio, Teri A. et al. “Implementing Genomic Medicine in the Clinic: The Future Is Here.” Genetics in Medicine 15.4 (2013): 258–267. PMC. Web. 21 Sept. 2018. 6. https://www.cancer.gov/about-cancer/causes-prevention/genetics
2. Delaney, Susan K. et al. “Toward Clinical Genomics in Everyday Medicine: Perspectives and Recommendations.” Expert Review of Molecular Diagnostics 16.5 (2016): 521–532. PMC. Web. 21 Sept. 2018.
3. Bryce, Alan H., et al. “Comprehensive Genomic Analysis of Metastatic Mucinous Urethral Adenocarcinoma Guides Precision Oncology Treatment: Targetable EGFR Amplification Leading to Successful Treatment With Erlotinib.” Clinical Genitourinary Cancer, vol. 15, no. 4, 2017, doi:10.1016/j.clgc.2016.11.001.
4. Torkamani, Ali et al. “High Definition Medicine.” Cell 170.5 (2017): 828–843. PMC. Web. 21 Sept. 2018.
5. Borad, Mitesh J. et al. “Clinical Implementation of Integrated Genomic Profiling in Patients with Advanced Cancers.” Scientific Reports 6 (2016): 25. PMC. Web. 21 Sept. 2018.
6. https://www.cancer.gov/about-cancer/causes-prevention/genetics