-
Harnessing the immune system to fight ovarian cancer
Mayo Clinic research is biomanufacturing an experimental, cell-based ovarian cancer vaccine and combining it with immunotherapy to study a "one-two punch" approach to halting disease progression in ovarian cancer patients.
This research begins with a blood draw from women with advanced ovarian cancer whose tumors have returned after standard surgery and chemotherapy. White blood cells are extracted from the blood, biomanufactured to become dendritic cells and are returned to the patient. Dendritic cells act as crusaders that march through the body, triggering the immune system to recognize and fight cancer.
"We're building on an earlier phase 1 clinical trial that showed promising results in terms of survival after the dendritic cell-based vaccine," says Matthew Block, M.D., Ph.D., co-principal investigator and medical oncologist. "Of the 18 evaluable patients in the phase 1 study, 11 had cancer return, but seven of them — 40 % — have been cancer-free for almost 10 years. We typically expect 90% of patients in this condition to have the cancer return."
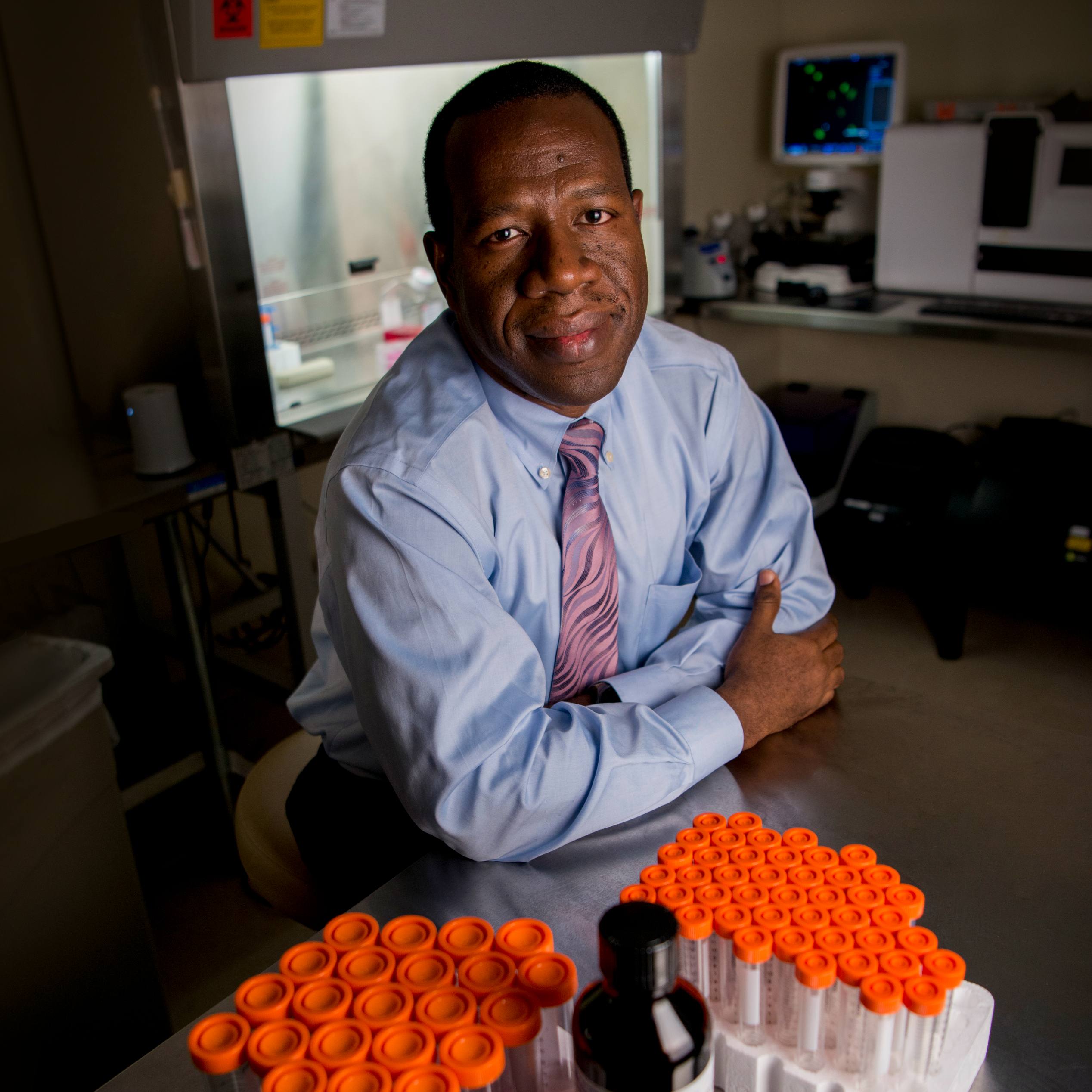
Mayo Clinic's pioneering approach, developed in the lab of Keith Knutson, Ph.D., equips the vaccine with bits of proteins that unleash an immune response. Specifically, the vaccine is targeted to harness Th17 immunity. In ovarian cancer, Th17 cells are linked to reduced immune suppression and improved survival. By driving a Th17 immune response, the vaccine aims to redirect the immune system's efforts to fight cancer.
"To our knowledge, nobody else has ever deliberately tried to make a Th17 immune response using a cancer vaccine. It targets a new part of the immune system that fights infection and activates a defense mechanism," says Dr. Knutson, co-principal investigator on the study. "We want to learn if that immune response is more helpful to ovarian cancer patients who have relapsed than other types of immune responses."
The vaccine will be given in combination with a checkpoint inhibitor immunotherapy drug to identify and kill stealthy tumors that don't respond to cell therapy alone. Preclinical research by Dr. Knutson's team in mouse models suggests that the combination of the immunotherapy drug and Th17-targeting vaccine creates a synergistic effect that strengthens the immune system's ability to target and kill ovarian cancer cells.
"What's exciting about this research is this allows us to study why tumors have recurred. We will investigate what turned on the immune response and what caused it to wane," says Dr. Block. "We hope to learn whether there is a complementary effect in which the two interventions work together better in ovarian cancer patients than either of them alone."
The aim of the vaccine is to prevent ovarian cancer tumors from returning. The latest research also seeks to understand why some ovarian cancer tumors evade the body's immune response. Relapsing cancer is often more aggressive and difficult to treat.
Biomanufacturing on-site a key to research
Biomanufacturing is a crucial step that advances promising research such as the dendritic cell vaccine from the lab to patient care. It involves preparing biological products to safely be given to patients in early-stage clinical trials.
Mayo Clinic's Center for Regenerative Biotherapeutics is leading the biomanufacturing efforts across all its campuses with a four-pillar approach that includes process development for mass production, quality control measures and quality assurance. This framework helps ensure the safety, identity, strength and purity required of commercial-grade medicines.
Clinical trials for cell-based ovarian cancer vaccines would be difficult, if not impossible, at Mayo Clinic without its biomanufacturing facilities. Once white blood cells are extracted from the patient, they must be transferred to the lab within hours to be grown and prepared for biomanufacturing.
"Manufacturing of an ovarian cancer vaccine is personalized and targeted to each patient's unique immune profile," says Dr. Knutson. "It is absolutely essential to our research to have biomanufacturing facilities on-site, near the patient, in case we need to make adjustments based on each patient’s individual tumor that could better kill cancer cells."
"That's what makes this research unique from a scientific standpoint. The study participant can walk over to the lab, have the blood drawn and within hours their specimen can be transferred to the on-site facility where the process of biomanufacturing the vaccine begins," says Dr. Block. "That would not be possible with an outside manufacturer."
A deadly form of reproductive system cancer
Ovarian cancer is the deadliest form of gynecologic cancer. It often is not diagnosed until advanced stages, when it is less treatable. Even with standard surgery and chemotherapy, tumors return in up to 70% of women. The outcome is often poor. 19,000 women in the U.S. are diagnosed with ovarian cancer every year and more than 13,000 die from it, according to the American Cancer Society.
Mayo Clinic will begin biomanufacturing the ovarian cancer vaccine for a phase 2 clinical trial in Rochester, with plans to expand the biomanufacturing capabilities to Florida and Arizona.
The results of the phase 2 clinical trial will determine whether the cell-based ovarian cancer vaccine will advance to later-stage biomanufacturing and clinical trials. Mayo hopes to then work with an industry collaborator to license the technology and bring it to market to expand patient access around the world.
Even with promising scientific evidence, it could take several years before the cell-based ovarian cancer vaccine is available for daily patient care, though investigators are hoping it will be sooner.
Mayo Clinic's Center for Individualized Medicine and Comprehensive Cancer Center also supported this research.
###