-
Featured News
Heart Brain Clinic individualizes care, treatment of unexplained stroke
 Each year in the U.S., more than 800,000 people suffer a stroke. And once patients have had a stroke, they are at risk for another. Preventing a subsequent stroke can be challenging, especially if the cause of the initial stroke is not known. To help in evaluate and treat patients with unexplained stroke, Mayo Clinic created the Heart Brain Clinic on Mayo Clinic's Florida campus.
Each year in the U.S., more than 800,000 people suffer a stroke. And once patients have had a stroke, they are at risk for another. Preventing a subsequent stroke can be challenging, especially if the cause of the initial stroke is not known. To help in evaluate and treat patients with unexplained stroke, Mayo Clinic created the Heart Brain Clinic on Mayo Clinic's Florida campus.
"Cryptogenic stroke accounts for 20–30 percent of all ischemic strokes, which translates to approximately 160,000 to 240,000 patients each year in the U.S.," says Dr. Michelle Lin, a Mayo Clinic neurologist and co-director of the Heart Brain Clinic. "The condition is especially common in young patients who have no other identifiable symptoms or risk factors for stroke."
"The Heart Brain Clinic is a place where patients come and gain the benefit of a team. They are seen by a cardiologist and a neurologist in the same visit to determine what caused their stroke and how best to treat them," explains Dr. Peter Pollak, a Mayo Clinic interventional cardiologist and co-director of the Heart Brain Clinic.
Heart disease, including atrial fibrillation, heart attack, heart failure and valvular disease increases the risk of stroke due to embolism. Undiagnosed atrial fibrillation or a congenital heart defect known as a patent foramen ovale (PFO) are common triggers for many stroke patients. "The collaborative nature of the Heart-Brain Clinic allows us to determine whether patients with heart disease will benefit from surgery or medical treatment to prevent stroke or hemorrhage," says Dr. Lin.
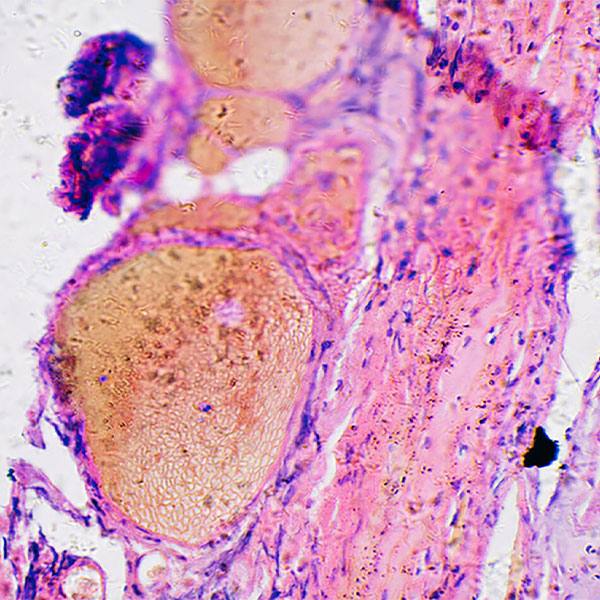
A patent foramen ovale affects almost 2 billion people around the world, says Dr. Pollak. For about 1 in 4 people, the flap between the two top chambers of the heart — the right atrium and the left atrium — does not seal properly at birth. Many people may never know they have a patent foramen ovale, he says.
"It's normally not a problem, except some people may form a clot in their venous system that may travel to the arterial system when they cough, throw up or bear down. This clot can form a stroke if it blocks an artery in the brain," says Dr. Pollak.
"If you've had a stroke and you're found to have a PFO, I think it is really important to see a collaborative clinic with a neurologist and a cardiologist to figure out whether your PFO was really the culprit and whether closing the PFO will reduce the likelihood of recurrent stroke, of another event," says Dr. Pollak.
The Heart Brain Clinic also sees many patients diagnosed with atrial fibrillation, a heart rhythm disorder where the atria beat irregularly and chaotically. Atrial fibrillation decreases the heart's blood-pumping efficiency and increases a patient's stroke risk.
"We believe that risk comes from clots that may form in a corner of the heart called the "left atrial appendage." For most patients, treatment with blood-thinning medicines has been found effective to prevent a clot from forming in that corner and potentially causing a stroke," explains Dr. Pollak.
However, some people cannot tolerate blood thinners or they have other issues that may lead doctors to recommend implanting a small device to close the left atrial appendage.
"The Watchman device reduces stroke risk without increasing bleeding risk long term that occurs if they were on blood-thinning medications," says Dr. Pollak.
"We want to help our patients reduce their risk for recurrent stroke. The collaborative nature of the Heart Brain Clinic allows for real-time shared decisions that are individualized to each patient to prevent recurrent strokes," says Dr. Lin.