-
Cancer
Hepatic artery infusion pump therapy for colorectal liver metastases
When facing colorectal liver metastases or colorectal cancer that has spread to the liver, finding effective treatment options can be challenging. Dr. Katherine Poruk, a surgical oncologist at Mayo Clinic, says a specialized therapy known as hepatic artery infusion pump (HAIP) chemotherapy is an option for some.
Watch: Dr. Katherine Poruk explains hepatic artery infusion pump therapy
Journalists: Broadcast-quality sound bites with Dr. Poruk are available in the downloads at the end of the post. Please courtesy: "Mayo Clinic News Network." Name super/CG: Katherine Poruk, M.D./Surgical Oncology/Mayo Clinic.
What is HAIP therapy?
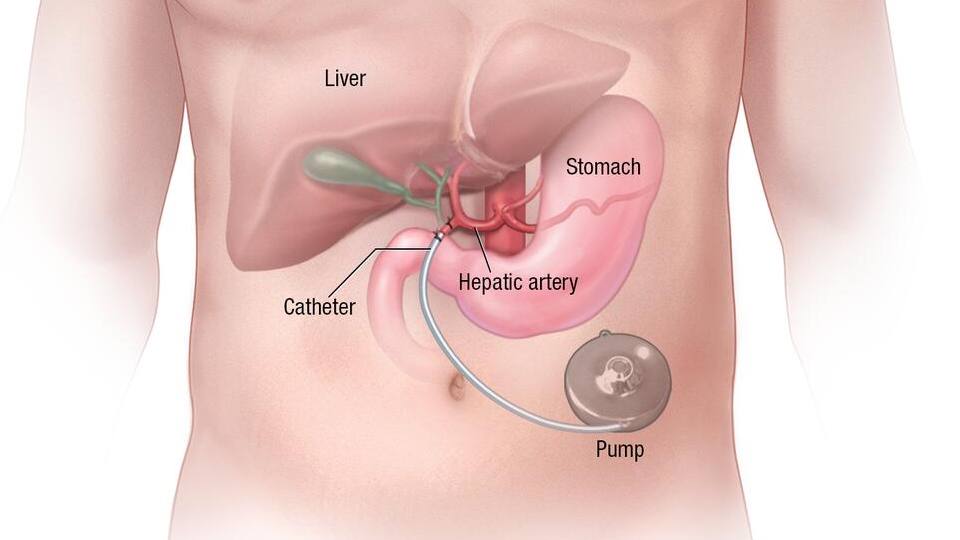
HAIP therapy targets tumors specifically in the liver, whether they are primary liver cancers or cancers that have spread from other parts of the body, most commonly the colon. The process begins with the surgical implantation of a small pump under the skin, typically in the abdomen.
This pump acts as a reservoir for chemotherapy, which is delivered directly to the liver through a catheter placed in the hepatic artery — the main artery supplying blood to the liver.
"The benefit of HAIP therapy is that it provides a very high dose directly to the liver, allows the chemotherapy to stay there, and can prevent some of the systemic therapy side effects that patients often experience," explains Dr. Poruk.
This method allows for much higher doses of chemotherapy than standard treatments. The liver receives the full force of the medication, while the rest of the body avoids common
chemotherapy side effects such as nausea, vomiting and fatigue.
Who benefits from HAIP therapy?
"Patients who have liver metastases from a colorectal tumor that are not amenable to surgery or other local therapies, we find that these patients would benefit from pump therapy, as it can help to downstage the tumors and potentially treat them. And this is true whether or not they're responding to systemic chemotherapy," says Dr. Poruk.
Patients who have already undergone surgery to remove liver tumors also may benefit from HAIP. In these cases, HAIP is used after surgery to deliver chemotherapy directly to the liver, reducing the risk of cancer coming back. It also can help patients who haven't responded well to traditional chemotherapy.
"HAIP therapy does not close any doors, but can potentially open new avenues of treatment," she says.
What to expect during the procedure
HAIP is a surgical procedure that many patients find manageable, says Dr. Poruk. During surgery, a small pump, roughly the size of a hockey puck, is implanted under the skin, usually on the right side of the abdomen. The surgeon makes an incision, locates the hepatic artery, and inserts a catheter that connects the pump to the artery. This operation can be done either open or minimally invasive, depending on the patient. Once in place, the pump continuously delivers chemotherapy directly to the liver, where it can attack cancer cells more aggressively.
The pump remains in the body as long as chemotherapy is needed, typically for at least six months. After treatment is completed, the pump can be removed, although many patients continue with it if there is evidence of disease.
"The pump is very discreet under clothing, and most patients can wear clothes normally without anyone knowing they have it," explains Dr. Poruk.
Improving quality of life
One of the most significant advantages of HAIP is its improvement in quality of life for patients compared to traditional chemotherapy. While chemotherapy affects the entire body, HAIP localizes treatment to the liver.
"Patients who undergo HAIP therapy are often very happy with their results and are surprised at the ease of surgery and how well they feel despite undergoing high doses of chemotherapy," she says.
Less side effects means patients can often maintain their daily routines with fewer interruptions.
The goal of HAIP, says Dr. Poruk, is not just to manage cancer but to potentially lead to a cure. Patients who were previously not candidates for surgery may find their tumors shrinking enough to be surgically removed, giving them a chance at long-term remission or even cure.
"This can help shrink the tumors and allow patients to undergo either curative surgery or potentially even a liver transplant," she says.







