-
Improved treatments available for lymphedema patients
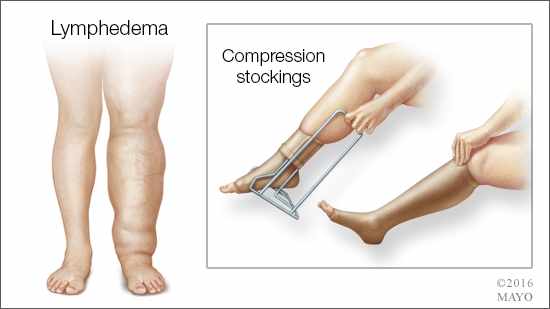 Arm or leg swelling, fluid retention and skin infections are common among cancer patients who have had surgery on or radiation to their lymphatic network. The condition, known as lymphedema, occurs when there is an accumulation of lymphatic fluid in the upper or lower extremity because the lymphatic vessels are unable to drain adequately.
Arm or leg swelling, fluid retention and skin infections are common among cancer patients who have had surgery on or radiation to their lymphatic network. The condition, known as lymphedema, occurs when there is an accumulation of lymphatic fluid in the upper or lower extremity because the lymphatic vessels are unable to drain adequately.
“For many people, lymphedema is synonymous with breast cancer but the condition can affect people treated for other cancers, including sarcoma, melanoma, prostate, testicular or gynecologic cancers and head and neck cancers,” says Dr. Sarah McLaughlin, surgeon and director at the Robert and Monica Jacoby Center for Breast Health at Mayo Clinic's campus in Jacksonville, Florida.
Symptoms can vary. In addition to swelling in parts of the arms or legs, lymphedema can cause a feeling of heaviness and infections and thickening of the skin. There can be complications due to this condition including bacterial infections and lymphangiosarcoma, a rare form of soft tissue cancer that is caused by untreated lymphedema.
Lymphedema has no cure, but the condition can be managed, especially if caught early, says Dr. McLaughlin. “We know that, if we can identify the swelling early and intervene early, treatment may be easier and more effective for patients. Unfortunately, it cannot be cured.”
Who is at risk?
The risk of developing the condition varies based on the type of surgery performed, says Dr. McLaughlin.
Approximately 20 percent of all breast cancer patients develop lymphedema, she estimates, but notes that the true incidence of lymphedema is not entirely known, in part because it might not develop for monthsor years after treatment.
“This condition doesn’t happen immediately after surgery. It can take anywhere from six months to three years, so it’s hard to know who is actually going to get it, and it is not always reported,” says Dr. McLaughlin.
For example, breast cancer patients who require a sentinel node biopsy with approximately two to four lymph nodes removed have an estimated 5 percent risk of developing lymphedema, Dr. McLaughlin says. The risk increases to between 15 and 20 percent for women with more invasive disease who require most or all of their underarm lymph nodes to be removed, she says.
Quality of life impacts
While some patients may only experience limited swelling, lymphedema is a chronic condition requiring daily treatment to reduce and manage pain and swelling. Patients typically require specialized physical therapy, skin care and massage, as well as customized compression garments.
“Lymphedema negatively impacts a patient’s quality of life for the duration of his or her life, in part, because of the necessary care and maintenance to manage his or her condition. As the lymphedema progresses, it becomes more burdensome for patients,” Dr. McLaughlin explains.
Advances in treatment
Recent surgical advances have made surgical management of lymphedema a viable alternative.
“Mayo Clinic’s campus in Florida is one of a few centers in the country offering patients a minimally invasive surgery, known as lymphovenous bypass, which has been shown to significantly improve a patient’s quality of life,” says plastic and reconstructive surgeon Dr. Antonio J. Forte.
“Though surgery is not curative, microsurgical treatment of lymphedema allows patients to have great improvement of their condition by removing the excessive fluid that accumulates in their limbs,” Dr. Forte explains.
With this technique, a few small incisions are made just underneath the skin in the arm. Then, using a microscope, the surgeon connects a lymphatic vessel with a small vein to bypass the blockage and allow the excess fluid to drain properly.
Dr. Forte says that, while most of his patients report dramatic improvements in their day-to-day life following the bypass, some swelling still occurs.
MEDIA CONTACT: Cynthia Weiss, Mayo Clinic Public Affairs,
507-284-5005, newsbureau@mayo.edu
Watch: Dr. Forte & Dr. McLaughlin talk more about lymphedema.
Journalists: Broadcast-quality sound bites with Dr. Forte are in the downloads.
Ongoing work and education
Dr. McLaughlin is leading additional research studies focused on lymphedema, with the goal of identifying patients who are at risk for the condition and then helping them manage the disorder, so they can maintain a positive quality of life.
“Many women worry about lymphedema and then alter their lifestyle because of their worry and anxiety about developing it. It is important that we educate all of our patients on their risk of lymphedema and create tailored interventions and prevention strategies for each woman. We don’t want them to live the rest of their life in fear.”