-
Cancer
Improving outlook for pancreatic cancer
 "Advances in screening, surgery and genetic classification are leading to improvements for treating pancreatic cancer." - Dr. Michael Wallace
"Advances in screening, surgery and genetic classification are leading to improvements for treating pancreatic cancer." - Dr. Michael Wallace
November 17 is World Pancreatic Cancer Day but the entire month of November is meant to bring awareness to this disease. Although the incidence of pancreatic cancer has not risen significantly over the past decade, the disease is the third most common cause of cancer death in the United States, recently surpassing breast cancer. According to the National Cancer Institute, 53,000 new cases of pancreatic cancer are expected in 2016, but an estimated 42,000 deaths will occur annually.
“Although we have made great advances in many cancers, pancreas cancer remains one of the most difficult to treat ― often because patients are diagnosed at a late stage,” says Dr. Michael Wallace, a gastroenterologist on Mayo Clinic’s campus in Jacksonville, Florida. “But I am optimistic about the future, as we are seeing major areas of progress.”
Advances in screening for high-risk individuals, surgical innovations and new genetic classifications are changing the outlook for pancreatic cancer, he says.
High-risk populations
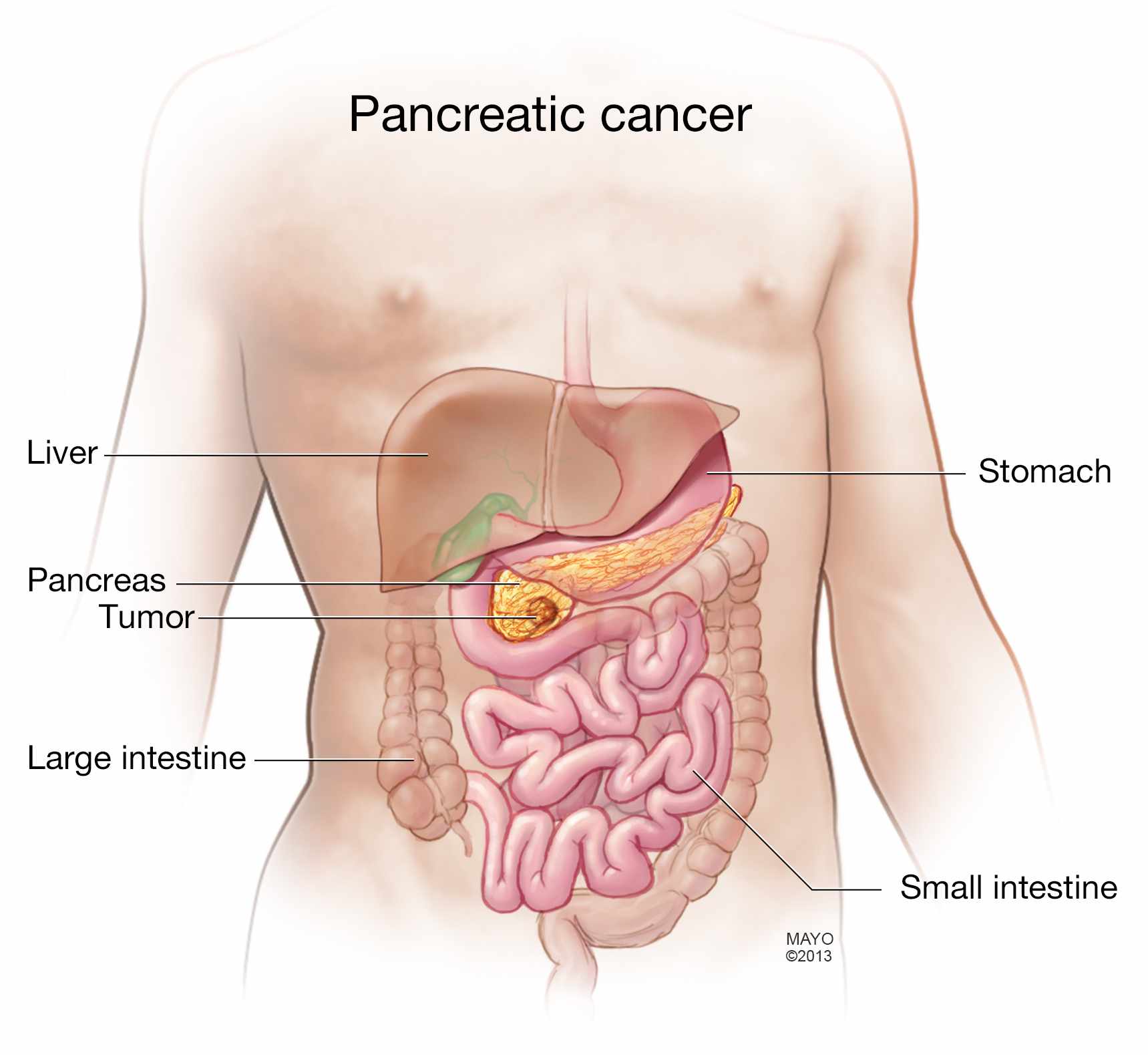
Pancreatic cancer begins in the tissues of your pancreas — an organ in the abdomen that secretes enzymes to aid digestion and hormones to help regulate the metabolism of sugars. All individuals, regardless of gender, race, color or age, can be at risk, says Dr. Wallace. Heavy alcohol use, coupled with heavy tobacco use increases risk.
Although there are several known pancreatic cancer syndromes – fewer than 1 in 10 people have a known genetic risk factor, he says. But individuals who have one or more family members affected by pancreatic cancer, especially at a young age, should be monitored.
“This broad group of people may represent up to 20 percent of individuals who are at increased risk, but it is important that we follow them closely, especially since we do have effective screening tests now, including MRI and endoscopic ultrasound,” he notes.
Cysts and risk
Thanks to advances in MRI technology, doctors today can identify pancreatic cysts, small saclike pockets of fluid that may increase the risk for cancer. “We find cysts in about 40 percent of the population. While most are inconsequential, it is important to distinguish which of them are benign and which we need to either watch, biopsy or even surgically remove,” Dr. Wallace explains.
In 2015, Dr. Wallace and a team of colleagues developed a profile of the patient who would be most at risk of these lesions developing into cancer. Their analysis was published in Digestive and Liver Diseases.
Journalists: Sound bites with Dr. Wallace are in the downloads.
https://youtu.be/nSa2VWTLUm4
“Studies such as these allow us to further stratify people into a low-, medium- or high-risk category for their cyst becoming cancerous, based on characteristics, including size and shape. This will hopefully enable us to help diagnose cancer earlier and, in turn, positively impact survival,” he says.
Surgical and genetic advances
“Traditionally, only about 5 percent of all patients are diagnosed at an early stage where we can resect their tumor completely with surgery,” Dr. Wallace says. “Now, we are pushing the boundary of who we can get to surgery. Because, if we can get the tumor out, we can cure those individuals.”
In addition, robust research related to the genetic classification of tumors is helping to evolve treatment for many patients.
In the past, genetic information was usually only available from surgical specimens. But, today, thanks to fine needle biopsies, “we’re able to get enough material and look at genetic sequences to see if there is a better medication available when our current options are exhausted,” Dr. Wallace explains.
“Precision medicine is very exciting, but we’re seeing major areas of progress on many fronts for pancreatic cancers,” says Dr. Wallace. “There is hope for this cancer.”







