-
Featured News
Infectious Diseases A-Z: Understanding antibiotic resistance during World Antibiotic Awareness Week
Penicillin is a powerful antibiotic that has saved millions of lives since its discovery in 1928. Now, 90 years later, overuse of this and other antibiotics has led to antibiotic resistance.
“The resistance that’s happening in bacteria due to inappropriate or unnecessary use of antibiotics has led to a global and national health threat,” says Dr. M. Rizwan Sohail, a Mayo Clinic infectious diseases specialist.
It's not the human body that becomes resistant to antibiotics. It's the bacteria that get resistant. "As bacteria are exposed to more antibiotics, the bacteria evolve and change. What happens next is antibiotics are unable to kill those bacteria when we really want them to," says Dr. Sohail.
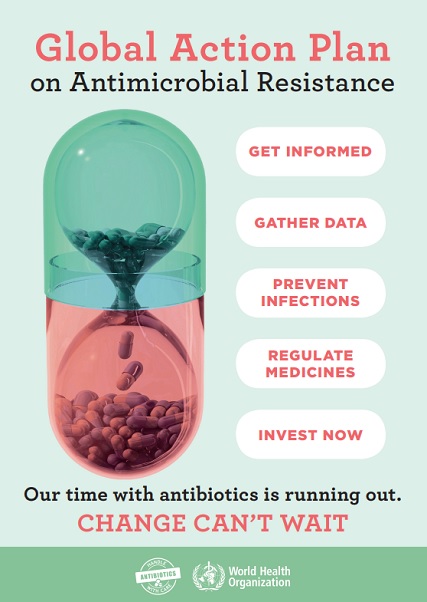
Antibiotic resistance has led to illness and death. “Each year, according to the World Health Organization, approximately 700,000 people around the globe die of bacterial infections that are resistant to antibiotics. In the U.S, the Centers for Disease Control and Prevention estimates that nearly 2 million Americans get infection with bacteria that are antibiotic resistant – resulting in approximately 23,000 deaths in the U.S. each year,” says Dr. Sohail.
Watch: Dr. Rizwan Sohail discusses antibiotic resistance.
Journalists: Broadcast-quality sound bites with Dr. Rizwan are in the downloads at the end of the post. Please ‘Courtesy: Mayo Clinic News Network.’
During this World Antibiotic Awareness Week Nov. 12 – 18, Dr. Sohail answers Mayo Clinic News Network questions below, about the overuse of these powerful medications:
What do antibiotics work for and against?
“Antibiotics work against bacteria,” says Dr. Sohail. “They do not work against viruses, or parasites or mold infections. A lot of the upper airway infections, such as sinus infections, ear infections, or bronchitis that people come to visit their doctors for in the clinic or in the ED [Emergency Department], are caused by viruses. And, therefore, the antibiotics don’t really help in these situations.”
Can one person make a difference in the fight against antibiotic resistance?
“Everybody needs to play their role. As physicians or healthcare providers, we need to be more careful about choosing the right antibiotic to treat bacterial infections.” Dr. Sohail adds, “As patients or family members, we need to be aware of the side effects of antibiotics, and should not insist on getting the antibiotics if our doctor does not think they would help us.”
What are specific things each of us can do to help with the problem?
“Stay healthy ourselves, and practicing hand hygiene can limit the spread of infection from us to others. Also, patients or their parents should not share the antibiotics. They should always ask their health care providers if they need antibiotics because they may not be helpful. When we do get the antibiotics, we should take them as prescribed, at the appropriate time, and for the appropriate duration. Do not take your antibiotics longer, or not even shorter than the time that was recommended by the physicians, or provider,” says Dr. Sohail.
Related post:
Can you pass the penicillin allergy quiz?







