-
Intensive Treatment of Glucose Levels Can Lead to Serious Complications
 ROCHESTER, Minn. — With a more-is-better mindset common in society, frequent commercials encouraging checks of glycated hemoglobin (HbA1C) levels, and ads for new diabetes medications to lower HbA1C in adults with Type 2 diabetes, Mayo Clinic researchers were not too surprised to find overtesting occurring.
ROCHESTER, Minn. — With a more-is-better mindset common in society, frequent commercials encouraging checks of glycated hemoglobin (HbA1C) levels, and ads for new diabetes medications to lower HbA1C in adults with Type 2 diabetes, Mayo Clinic researchers were not too surprised to find overtesting occurring.
Beyond overtesting, however, such focus on HbA1C levels can lead to serious harms for patients, reports the research team, especially as more diabetes medications are needed to keep HbA1C within desired targets. This is particularly important for older patients with other medical conditions, they report in a new study, published online on June 6 in JAMA Internal Medicine.
“At first, we were surprised to find how much overtesting for HbA1C is occurring among adults of all ages with Type 2 diabetes who were already well-controlled,” says Rozalina McCoy, M.D., a Mayo Clinic primary care physician and endocrinologist, and lead author of the study. “But, then, we realized that not only were patients being tested frequently, they were also being treated with more medications than we would expect considering how low their HbA1C already was. So, this led us to do this study ─ to see how frequently patients are treated so intensively that they may be overtreated and what that does to their risk of hypoglycemia.”
“In this study, we found that, particularly among older patients and patients with serious chronic conditions, intensive treatment nearly doubled the risk of severe hypoglycemia requiring medical attention, including hospitalization,” says Dr. McCoy.
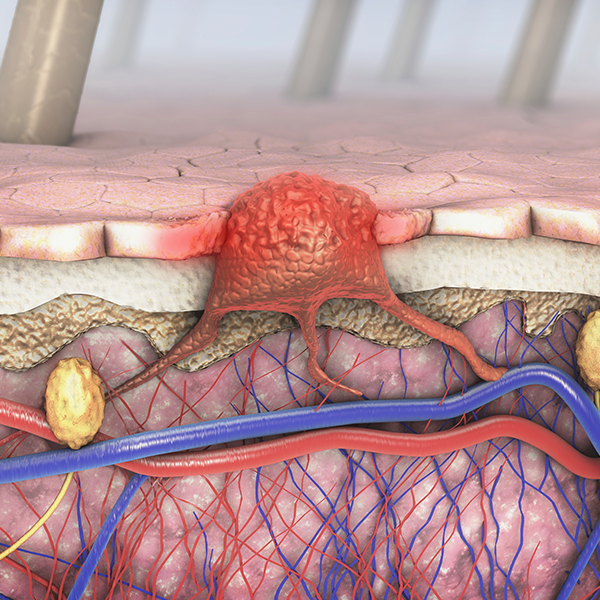
Hypoglycemia is a serious potential complication of diabetes treatment. It worsens quality of life and has been associated with cardiovascular events, dementia and death.
Most professional societies recommend targeting HbA1C levels less than 6.5 or 7 percent, with individualized treatment targets based on patient age, other medical conditions, and risk of hypoglycemia with therapy.
“Treating patients to very low HbA1c levels is not likely to improve their health, especially not in the short term, but can cause serious harms, such as hypoglycemia,” says Dr. McCoy.
MEDIA CONTACT: Robert Nellis or Elizabeth Zimmermann Young, Mayo Clinic Public Affairs, 507-284-5005, newsbureau@mayo.edu
For the purposes of this study, “intensive treatment” was defined as being treated with more glucose-lowering medications than clinical guidelines consider necessary given a patient’s HbA1C level. Patients whose HbA1C was less than 5.6 percent (Diabetes is defined by HbA1C 6.5 percent or higher.) were considered intensively treated if they were taking any medications. Patients with HbA1C in the prediabetes range, 5.7-6.4 percent, were considered to be intensively treated if using two or more medications at the time of the test, or if started on additional medications after the test, because current guidelines consider patients with HbA1C less than 6.5 percent to be optimally controlled already. For patients with HbA1C of 6.5-6.9 percent, the sole criteria for intensive treatment was treatment intensification with two or more drugs or insulin.
The researchers examined medical claims, pharmacy and laboratory data of 31,542 adults with stable and controlled Type 2 diabetes who were included in the OptumLabs Data Warehouse between 2001 and 2013. None of the patients were treated with insulin or had prior episodes of severe hypoglycemia ─ both known risk factors for future hypoglycemic events. None of the patients had obvious indications for tight glycemic control, such as pregnancy.
“Our goal was to specifically assess the degree to which intensive treatment – not other known risk factors, such as prior hypoglycemic events or insulin therapy – caused hypoglycemia,” says Dr. McCoy. “We also wondered if young and healthy patients may be better able to tolerate intensive treatment than older patients or those with complex medical problems, so we specifically looked at the impact of intensive treatment on these two groups separately.”
Therefore, the patients were separated by whether they were considered clinically complex, as defined by the American Geriatrics Society: 75 years or older; having end-stage kidney disease or dementia; or having three or more serious chronic conditions. This distinction has been made to help identify patients for whom adding glucose-lowering medications is more likely to lead to treatment-related adverse events, including hypoglycemia, while not providing substantial long-term benefit.
Of the 31,542 patients in the study, 18.7 percent of clinically complex patients and 26.5 percent of non-complex patients were treated intensively. Clinically complex patients had nearly double the rate of severe hypoglycemia than non-complex patients, and intensive treatment increased it by an additional 77 percent, from 1.74 to 3.04 percent over two years.
According to Dr. McCoy, “This means that 3 out of 100 older or clinically complex patients with diabetes who never had hypoglycemia before, whose HbA1C is within recommended targets, and who are not on insulin, will experience a severe hypoglycemic episode at some point over two years.”
“This does not even capture the more mild episodes of low blood sugar that patients can treat at home, without having to go to the doctor, emergency department or hospital,” she says.
“These findings are concerning for many reasons,” says Dr. McCoy. “Overtreatment results in greater patient burden, higher risk of medication side effects, and more severe hypoglycemia, which can lead to serious injury and even death. It adds more unnecessary costs for patients and the health care system. And, at the same time, there is often little or no benefit from such intensive treatment ─ not in the long term and certainly not in the short term.”
“As clinicians, we need to understand not only what tests and medications are necessary, but also determine which ones are not, and which ones may cause more harm than good,” she says. “We need to individualize treatments to the needs and goals of our patients, and be comfortable saying ‘sometimes, doing less is ultimately giving our patients more.’ My hope is that others will be able to apply our findings in their practices for the benefit of patients everywhere.”
Other members of the collaborative research team are:
- Kasia Lipska, M.D., Yale University School of Medicine
- Xiaoxi Yao, Ph.D., Mayo Clinic
- Joseph Ross, M.D., Yale University School of Medicine
- Victor Montori, M.D., Mayo Clinic
- Nilay Shah, Ph.D., Mayo Clinic, OptumLabs
This research, which was made possible by the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery, used the OptumLabs Data Warehouse (OLDW). The OLDW includes claims data from more than 130 million commercially insured and Medicare Advantage enrollees of all ages and races, from all 50 states. It is a resource of OptumLabs, a collaborative research and innovation center cofounded by Mayo Clinic and Optum in 2013. This large data source enables the researchers to investigate across a much broader patient base than previously available to health science researchers, resulting in more definitive findings.
The Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery leads that relationship for Mayo Clinic and has published a number of studies identifying areas for potential improvements in health care delivery using the OLDW.
###
About Mayo Clinic
Mayo Clinic is a nonprofit organization committed to clinical practice, education and research, providing expert, whole-person care to everyone who needs healing. For more information, visit http://www.mayoclinic.org/about-mayo-clinic or https://newsnetwork.mayoclinic.org/.