-
Clinical Trials
Mayo Clinic, Carnegie Mellon researchers secure ARPA-H award for multiyear implantable device research for diabetes and obesity
Research teams from Mayo Clinic in Florida and Carnegie Mellon University will work on a federally funded project to accelerate the development and testing of a new device to treat patients with type 2 diabetes and obesity.
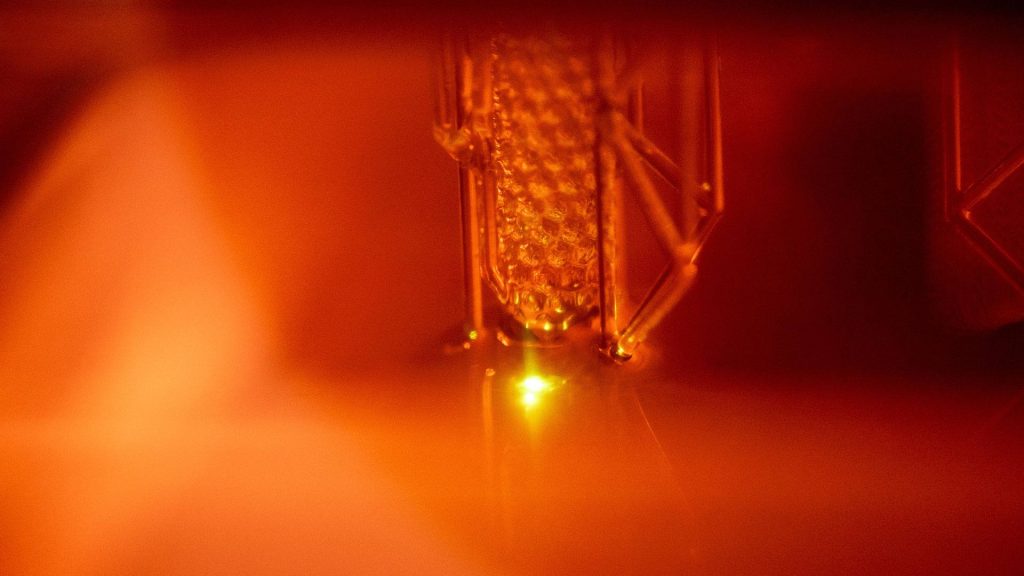
The bioelectrical device, known as Rx On-site Generation Using Electronics, or ROGUE, is being developed at Carnegie Mellon University. It will act as a "living pharmacy" using engineered cells capable of producing therapy to treat patients with both conditions. At the conclusion of device development, Mayo Clinic will conduct a first-in-human clinical trial to test the viability of ROGUE in humans for wider applicability.
The goal for the device is to produce regulated levels of glucagon-like peptide 1 (GLP-1)-based therapies, which can improve glucose levels in patients with diabetes and also promote weight loss.
The Advanced Research Projects Agency for Health, or ARPA-H, made the award to Carnegie Mellon and the project's principal investigator, Itzhaq Cohen-Karni, Ph.D. The ROGUE collaboration also includes bioengineering faculty from Boston University, Georgia Institute of Technology, Northwestern University, Rice University, University of California Berkeley and Bruder Consulting and Venture Group.

"There is great potential for ROGUE to expand access and decrease the costs of these medical therapies for at-risk patients who may not otherwise be able to use these agents for diabetes and obesity," says Susan Samson, M.D., Ph.D., chair of the Division of Endocrinology, Diabetes and Metabolism, Department of Medicine, Mayo Clinic in Florida. Dr. Samson has a background in preclinical models and translational research in the use of GLP-1 receptor agonists for metabolic disorders and is the clinical team lead and principal investigator of the project at Mayo.
ROGUE is an implanted device designed to make biological drugs more accessible to patients by reducing development and manufacturing costs while making it easier for patients to follow their treatment plan. The device, implanted during a minimally invasive outpatient procedure, will be designed to deliver continuous therapeutic peptides.

"Our team will be engaged throughout the project to provide expertise from the clinical side to ensure that the device is usable, safe and comfortable for patients down the line," says Mayo physician-scientist and co-principal investigator Maria Daniela Hurtado Andrade, M.D., Ph.D. Dr. Hurtado Andrade brings basic science and clinical trial expertise to the project and also is an expert in the field of weight management.
A phase one clinical trial will be conducted at Mayo Clinic in Florida, the sole clinical site for testing the device in humans. The trial requires the recruitment of a diverse group of patients, including those most at risk for diabetes and obesity.
"Mayo Clinic in Florida, which is embedded within the Jacksonville community, is strategically positioned to recruit this diverse study population," says Dr. Hurtado Andrade. As part of the project, Mayo Clinic will provide diabetes educators to help educate patients on the device's use.







