-
Featured News
Mayo Clinic discovers new role for protein to fight tumors
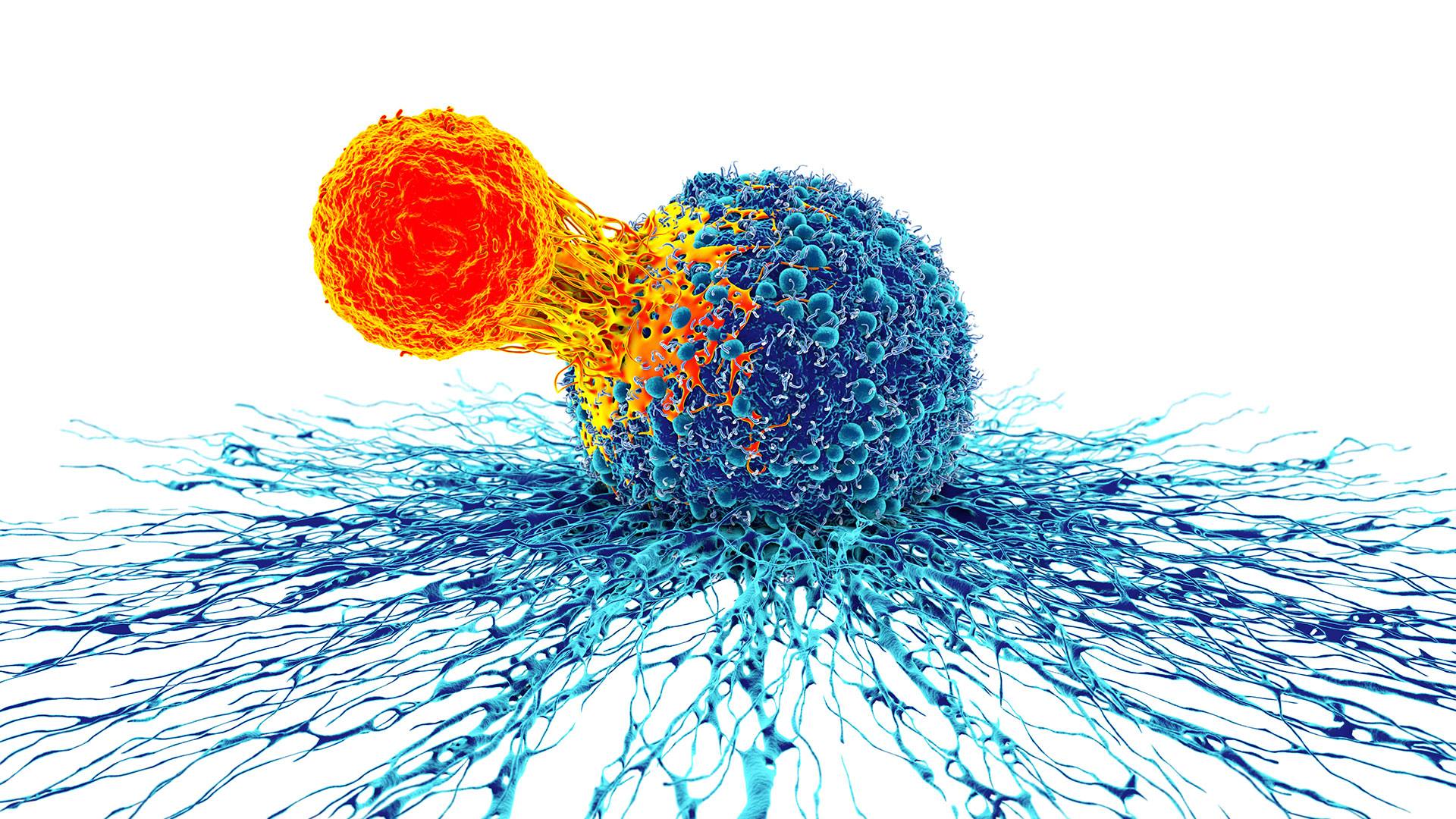
Mayo Clinic researchers have discovered a new role that a specific protein plays in regulating cell resistance and fighting tumors in certain types of cancer, offering hope for improved cancer therapies and patient outcomes.
The protein, known as NKG7, is found in CD8+ T cells, a type of immune cell that can recognize and kill cancer cells. CD8+ T cell resilience is essential for anti-tumor activity. The protein allows CD8+ T cells to continue killing cancer cells even under stress and can help prevent cancer from growing and spreading.
"We found that patients with invasive bladder cancer who had NKG7-expressing CD8+ T cells within their tumor had superior survival compared to patients without," says Dan Billadeau, Ph.D., senior author of the study, detailed in Nature Communications. "This discovery holds promise for manipulating CD8+ T cells — for example, CAR-T and tumor-infiltrating lymphocytes (TILs) — to combat cancer."
T cell-based immunotherapy is a developing field that treats many types of cancers. However, Dr. Billadeau explains that a significant problem in using these therapies is that many patients may experience a transient or short-term response followed by cancer progression.
There are two main types of T-cell-based therapies:
CAR T-cell therapy takes T cells from patients and modifies them to express a chimeric antigen receptor (CAR). CARs are proteins that recognize specific antigens on cancer cells, allowing the T cells to target and kill cancer cells more effectively.
TIL (tumor-infiltrating lymphocytes) therapy involves taking T cells from a patient's tumor and growing them in a lab. Then, the cells are returned to the patient in a higher dose.
NKG7 is a protein expressed in cytotoxic lymphocytes like CD8+ T cells and natural killer cells. A prior Mayo Clinic study had linked it to durable responses from anti-PD-1 immunotherapy in patients with melanoma, a skin cancer. However, the mechanism remained unclear.
Dr. Billadeau says that in this new work, the team investigated how the NKG7 protein might make CD8+ T cells more resilient and able to combat cancer cells more efficiently.

"We showed that NKG7 works at the lysosome, an organelle in the cell's cytoplasm, to restrain the overactivation of mTOR, a protein that regulates cell growth and which limits the persistence of functional CD8+ T cells," says Dr. Billadeau. "We discovered a role of NKG7 in the longevity of effector CD8+ T cells that are crucial in the control of cancer progression."
The manipulation of NKG7 expression can be used in CAR-T and TIL therapy to enhance their function and increase anti-cancer responses. The findings may also aid in cancer prognosis, as high NKG7 expression in CD8+ T cells in a tumor might correlate with a better clinical outcome. The NKG7 levels in CD8+ T cells in cancer tissues and peripheral blood may predict responses to immune checkpoint inhibitor therapy, another therapy that helps the immune system fight cancer, but this needs further validation.
Next steps
The team's work suggests that providing NKG7 proteins to various CD8+ T cell therapies, such as CAR-T and TIL, will give these T cell therapies a more resilient phenotype, leading to better patient outcomes. The team is working on several projects to add NKG7 to these therapies and test them in animal models. They are also performing studies in other cancers to use CD8+/NKG7+ T cells to predict survival and response to different cancer immunotherapies.
Review the study for a complete list of authors, disclosures and funding.







