-
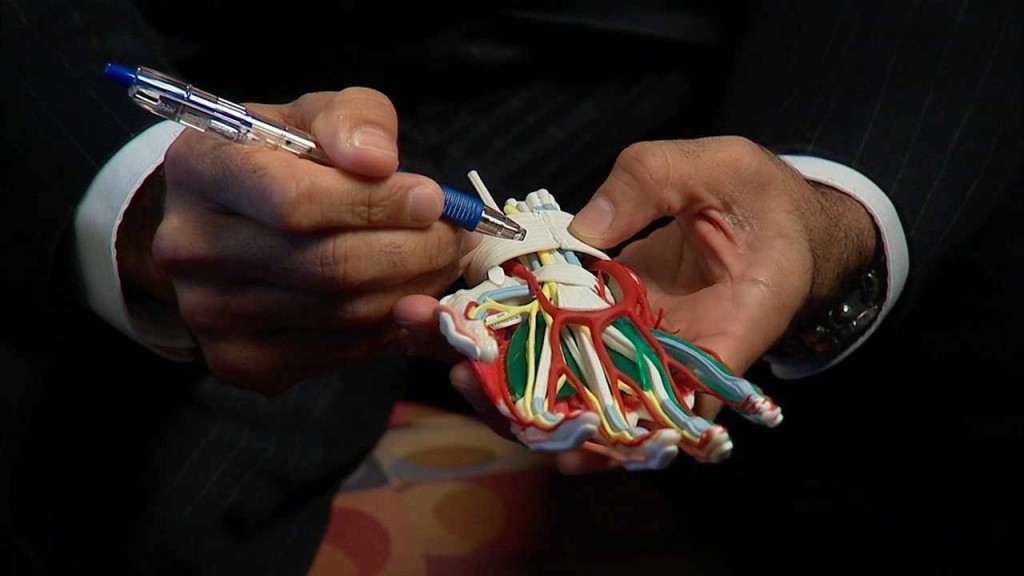
 Cardiovascular
CardiovascularMayo Clinic Health Letter: Highlights from the January 2015 Issue
ROCHESTER, Minn. ― Here are highlights from the January issue of Mayo Clinic Health Letter. You may cite this publication as often as you wish. Reprinting is allowed for a fee. Mayo Clinic Health Letter attribution is required. Include the following subscription information as your editorial policies permit: Visit https://healthletter.mayoclinic.com/ or call toll-free for subscription information, 1-800-333-9037, extension 9771. Full newsletter text: Mayo Clinic Health Letter January 2015 (for journalists only).
Wrist fractures: Treatment decisions not always straightforward
 Treatment decisions for wrist fractures quickly can become complicated, according to the January issue of Mayo Clinic Health Letter.
Treatment decisions for wrist fractures quickly can become complicated, according to the January issue of Mayo Clinic Health Letter.
The wrist is made up of eight small bones at the base of the hand and two in the forearm ― the radius and ulna ― that connect the elbow to the wrist bones. Any one of these bones can be fractured; a wrist fracture is a widely variable injury.
One of the primary decisions is the choice between nonsurgical and surgical treatment. Sometimes the choice is clear, and sometimes it’s not. Factors to consider include overall health, lifestyle, ability to tolerate surgery and the desire for a fully functioning wrist.
A simple wrist fracture, where the bone remains in position and is stable, often can be treated without surgery. A splint or cast is worn to maintain stability while the fracture heals.
A fracture that’s not aligned (displaced) sometimes can be aligned without surgery. In a process called closed reduction, lengthwise tension is applied to the arm and wrist, followed by manipulating the fracture into proper alignment. Local or other forms of anesthesia are used. If the closed reduction is successful and proper alignment is maintained, a splint and cast stabilize the bone while it heals.
Surgery to align and stabilize the fracture ― called open alignment ― is generally indicated when closed reduction doesn’t align the bone or keep it in place. In surgery, the fracture is stabilized with pins, rods, plates or screws. In addition, surgery often is indicated when the fracture extends into or disrupts the wrist joint.
Surgery or not?
For more complex fractures, surgery maximizes the odds of the best possible wrist function after healing. But, nonsurgical treatment means avoiding the possible complications of surgery including infection; nerve, blood vessel or tendon damage; difficulty with implanted hardware; or the need for additional surgery. With nonsurgical treatment, the fracture may not be optimally aligned. This can result in a loss of full motion or function of the wrist.
Deciding on the best treatment can be challenging, nuanced and worth a second opinion. For example, older adults who aren’t active might choose nonsurgical treatment ― and the potential loss of some wrist function ― to avoid surgery.
Recovery time will vary depending on overall health, severity of the fracture and any complications. It usually takes a bone six to eight weeks to heal. It may take a couple of months or up to a year for most joint stiffness to go away. Some level of stiffness or achiness may never go away.
Diuretics ― Effective and inexpensive option to treat high blood pressure
Diuretics, a class of drugs that have been available since the 1950s, continue to be a cornerstone therapy for high blood pressure. The January issue of Mayo Clinic Health Letter covers why treating high blood pressure (hypertension) is important and why treatment with diuretics has stood the test of time.
Hypertension is a disease where the pressure pushing blood through the arteries is high enough to gradually damage and stiffen normally elastic arteries throughout the body. It’s one of the leading causes of disability or death due to stroke, heart attack, heart failure, kidney failure and dementia. Lifestyle changes are the foundation of any treatment plan, but many people with hypertension also need medications.
Diuretics ― commonly referred to as water pills ― trigger the kidneys to excrete extra sodium in the urine. The sodium takes water and sodium from the blood. That decreases the amount of blood flowing through blood vessels, reducing pressure on the walls of the arteries and thus, blood pressure.
Effective new treatments have been developed to treat high blood pressure. They include angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), calcium channel blockers and others. However, research has repeatedly shown that appropriate diuretics reduce blood pressure and the risk of heart disease, stroke, heart attack, dementia and kidney disease as well or better than other drug classes. They are particularly effective in older adults and people of African descent.
Since diuretics have long since gone generic, they are typically the lowest cost drug choice. Diuretics are generally safe, but they can cause some side effects. Increased urination is the most common, but it is often temporary.
Keep exercising after joint replacement
The January issue of Mayo Clinic Health Letter offers do’s and don’ts for exercise after knee, hip or shoulder replacement.
Although it’s important to avoid too much wear and tear on a new prosthesis, low-impact activity is important for increasing bone density and fixing the prosthesis in place. In addition, improved muscle strength, balance and coordination resulting from regular exercise can help maintain and improve overall fitness and health.
Decisions about which activities to pursue depend on which joint was replaced and previous experience with activities. In general, recommended activities after joint replacement include those that don’t put too much stress on joints. High-impact activities such as contact sports, high-impact aerobics, racquetball, squash and other activities that involve a lot of running and jumping should be avoided.
The key to living well with a prosthetic joint is to find the right balance between rest and activity. Too much stress on the joint can cause harm. But too much inactivity can leave the muscles surrounding the joint weak, making movement difficult.
Mayo Clinic Health Letter offers some guidelines for activities that are considered OK, those that are OK with previous experience and those to avoid . Some examples include:
After hip replacement: Walking, stationary biking, low-impact aerobics, tai chi, gentle yoga, golfing and ballroom dancing are some of the activities that are considered OK. Weightlifting, road bicycling and ice skating are among the activities that are OK with previous experience. Singles tennis, racquetball, squash, jogging and running should be avoided.
After knee replacement: Walking, stationary biking, low-impact aerobics, tai chi, gentle yoga, golfing, horseback riding and bowling are some of the activities that are considered OK. Road biking, speed walking, doubles tennis and hiking are some of the activities that are OK with previous experience. Singles tennis, racquetball, squash, jogging and running should be avoided.
After shoulder replacement: Hiking, jogging or running, cross-country skiing, swimming using the breast stroke, aerobics, Pilates and tennis are considered OK activities. Racquetball and squash, baseball or softball, golfing, shooting and downhill skiing are considered OK with previous experience. Weightlifting, rock climbing and water skiing are not recommended.
###
Mayo Clinic Health Letter is an eight-page monthly newsletter of reliable, accurate and practical information on today’s health and medical news. To subscribe, please call 1-800-333-9037 (toll-free), extension 9771, or visit www.HealthLetter.MayoClinic.com.
MEDIA CONTACT: Brian Kilen, Mayo Clinic Public Affairs, 507-284-5005, newsbureau@mayo.edu







