-
Mayo Clinic Health Letter: Highlights from the March 2014 Issue
ROCHESTER, Minn. — March 21, 2014 — Here are highlights from the March issue of Mayo Clinic Health Letter. You may cite this publication as often as you wish. Reprinting is allowed for a fee. Mayo Clinic Health Letter attribution is required. Include the following subscription information as your editorial policies permit: Visit www.HealthLetter.MayoClinic.com or call toll-free for subscription information, 1-800-333-9037, extension 9771. Full newsletter text: Mayo Clinic Health Letter March 2014 (for journalists only).
Long QT syndrome ― Electrical Miscues in the Heart ― Can Cause Fainting, Seizures
 Long QT syndrome — when the electrical activity of the heart takes longer than it should to return to normal after a heartbeat — can lead to potentially dangerous heart rhythms. The March issue of Mayo Clinic Health Letter covers this condition and why it’s dangerous.
Long QT syndrome — when the electrical activity of the heart takes longer than it should to return to normal after a heartbeat — can lead to potentially dangerous heart rhythms. The March issue of Mayo Clinic Health Letter covers this condition and why it’s dangerous.
Long QT syndrome can cause fast, chaotic heartbeats that result in fainting, seizures or even sudden death. If long QT syndrome is suspected because of a fainting spell or family history, a doctor will likely suggest several tests, starting with an electrocardiogram (ECG).
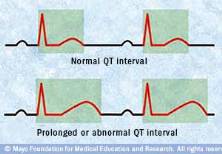
An ECG measures the heart’s electrical waves ― named after the letters Q through T ― and maps them to a graph to show the electrical activity in the heart’s lower chambers. The time between the start of the Q wave and the end of the T wave ― the QT interval ― is how long it takes for the heart to contract and then refill with blood. Sometimes an ECG conducted for another health condition is the first indication of long QT syndrome; many people with this syndrome have no noticeable symptoms.
A prolonged QT interval can be due to a genetic heart rhythm disorder. Unexplained deaths in children or young adults may be the first clue to an inherited long QT syndrome. The condition also can be acquired. Dozens of commonly used medications can lengthen the QT interval, even in otherwise healthy people. These medications include certain antibiotics, antidepressants, antihistamines and some that are used to treat diabetes. Medical conditions may cause long QT syndrome, too. They include eating disorders, illnesses that cause severe diarrhea or vomiting, some thyroid conditions and diabetes.
For congenital long QT syndrome, beta blockers are the first line of therapy. They slow the heart rate and make it less likely to go into dangerous rhythms. An implantable cardioverter-defibrillator (ICD) can stop potentially fatal arrhythmias, too. This device is considered for high-risk patients and those who have survived a long QT-triggered abnormal heart rhythm. Medication changes and other treatment options can improve acquired long QT syndrome.
Peripheral Artery Disease: When Heart Health Affects the Legs
The March issue of Mayo Clinic Health Letter covers why it’s important for older adults to have a blood pressure screening in the arms and legs at the same time.
The reason is peripheral artery disease (PAD). An estimated 15 to 20 percent of adults 70 and older have PAD, a condition that can cause leg pain or discomfort while walking and goes away with brief rest. Without treatment, PAD can worsen, resulting in leg pain occurring at rest, leg wounds that won’t heal, tissue death and even amputation.
The most common cause of PAD is hardening and narrowing of the arteries, a disease called atherosclerosis. These narrowed arteries reduce blood flow to organs and limbs. Risk factors include aging, smoking, diabetes, high blood pressure and undesirable levels of cholesterol.
Early symptoms of PAD often involve pain or discomfort in the legs, most commonly in the calf muscles, that reliably occurs after exercise or walking. The pain disappears after several minutes of standing. Other symptoms might include aching, heaviness, burning or just a sense of losing strength in the legs. Sensation can occur in the thighs, hip and buttocks, in addition to the calf muscles.
If PAD progresses, leg pain or discomfort may begin at rest and be intense enough to prevent sleep. Reduced blood flow can cause cold legs or feet, changes in skin color, sores on the legs or feet that won’t heal, and eventually tissue death, which may require amputation.
Only about half of people with PAD have symptoms, and others have vague symptoms, making the condition easy to overlook. That’s why PAD screening is recommended for adults age 65 and older and adults age 50 and older with a history of smoking or diabetes. Screening can be done in the doctor’s office by comparing blood pressure readings taken in the arms and legs.
Treatment involves strategies to improve cardiovascular health, such as quitting smoking, daily or near-daily exercise, and maintaining a healthy weight. To reduce pain, a doctor may recommend a supervised walking program that includes walking until pain occurs, resting, and walking again. This strategy helps condition muscles to use oxygen more efficiently. Improvements in length of time walking of 150 percent are common.
Surgery may be needed if improvements in cardiovascular health aren’t enough to slow the progression of PAD. Options include procedures to open narrowed arteries or bypass the blocked or narrowed arteries.
Unexplained Weight Loss Could be Digestive Malabsorption
Losing weight without diet or exercise changes could result from digestive malabsorption, the inability of the body to properly digest and absorb one or more nutrients. The March issue of Mayo Clinic Health Letter describes what occurs with this condition and how it can be treated.
Malabsorption can occur when any step in digestion is disrupted. Symptoms can include weight loss, chronic diarrhea or loose stools, more stool volume than usual, and abdominal bloating and gas. Excess fat in stools also is common, sometimes making stool seem pale, bulky, greasy, and extra foul-smelling. Other symptoms may be specific to deficiencies in certain vitamins. In older adults, signs and symptoms can be subtle and difficult to recognize.
Causes of malabsorption fall into two sometimes overlapping categories: difficulty with digestion and difficulty with absorption. Difficulty with digestion can be due to disease or damage to the pancreas or liver, an overgrowth of certain bacteria in the small intestine, or a deficiency in production of enzymes to break down lactose in dairy products, among others. Difficulty with absorption generally occurs when the small intestine is injured or damaged due to conditions that include celiac disease or Crohn’s disease. Infections, certain drugs and excessive alcohol consumption also can damage the small intestine.
Treatment depends on the underlying cause. Some causes such as disorders of the pancreas or bacterial overgrowth in the small intestine can be directly treated. Celiac disease or lactose intolerance can be treated with dietary changes. If underlying problems are not correctable, oral vitamin and mineral supplements may provide a sufficient boost to ward off deficiencies.
###
Mayo Clinic Health Letter is an eight-page monthly newsletter of reliable, accurate and practical information on today’s health and medical news. To subscribe, please call 1-800-333-9037 (toll-free), extension 9771, or visit www.HealthLetter.MayoClinic.com.
About Mayo Clinic
Recognizing 150 years of serving humanity in 2014, Mayo Clinic is a nonprofit worldwide leader in medical care, research and education for people from all walks of life. For more information, visit 150years.mayoclinic.org, www.mayoclinic.org and newsnetwork.mayoclinic.org.
MEDIA CONTACT:
Ginger Plumbo, Mayo Clinic Public Affairs, 507-284-5005, Email: newsbureau@mayo.edu