-
Cancer
Mayo Clinic Physicians Say High-definition Scopes Accurately Assess Polyps, Costly Pathological Examinations May Not Be Necessary
JACKSONVILLE, Fla. — It may not be necessary for experienced gastroenterologists to send polyps they remove from a patient’s colon to a pathologist for examination, according to a large study conducted by physician researchers at the Jacksonville campus of Mayo Clinic.

Their 522-patient study, published in the December issue of Gastrointestinal Endoscopy, found that physicians correctly evaluated whether a polyp was precancerous or benign using high-definition optical lenses during a colonoscopy. Their assessment was 96 or 97 percent accurate — depending on which of two generations of scopes was used — compared with a standard pathological evaluation of the polyps.
The Mayo Clinic researchers conclude that the pathological polyp examination now required by national practice guidelines may not be necessary — an advance they say could result in substantial cost savings for the patient and the health care system, as well as more rapid information and recommendations for follow-up for the patient.
“A colonoscopy is a fairly expensive procedure, and a large portion of the cost is the pathological analysis of polyps that are removed to check whether they are precancerous or benign — a check that determines when a patient needs another colonoscopy,” says the study’s senior investigator and gastroenterologist, Michael Wallace, M.D., MPH.
“We discovered that gastroenterologists using high-definition optical scopes can provide excellent care and diagnoses of polyps without the added step of a pathological examination,” Dr. Wallace says.
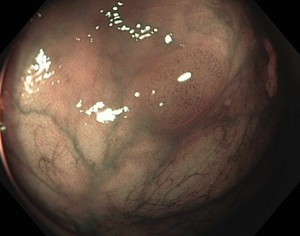
The research team examined use of the Exera II 180 colonoscope and the Exera III 190 colonoscope to assess 927 polyps. Both are high-definition scopes, and the earlier generation (180) is in wide use.
An optical diagnosis, sometimes referred to as a “virtual biopsy” was sufficient, in the hands of the experienced physicians, to determine that benign (hyperplastic) polyps were indeed benign, and that potentially precancerous (adenoma) polyps were the ones at risk for cancer development.
Investigators also found that physicians in the study had an extremely high adenoma detection rate using the scopes — 50 percent for the 180 model and 52 percent for the 190. “A high adenoma detection rate is considered a good measure of a quality colonoscopy. Studies have shown that a rate of 33 percent — meaning that of 100 people who undergo a colonoscopy, adenomas are found in 33 percent — is excellent,” says Dr. Wallace. “Current national benchmarks recommend an adenoma detection rate of at least 20 percent. We found substantially more adenomas.”
“The more adenoma polyps that are detected, the lower the risk is of getting colon cancer. So this study shows that it is possible to use an optical scope to perform a highly accurate colonoscopy and bypass the pathology laboratory, reducing cost,” he says. “Another advantage is that we can tell the patient immediately after the procedure what we found and when the next examination should be done, as opposed to waiting one to two days for a pathology result.”
The Mayo study is now being used by the American Society for Gastrointestinal Endoscopy to review current colonoscopy guidelines to assess whether or when pathological examination of polyps is necessary, he says.
The study was funded by Olympus Corporation of America, a manufacturer of endoscopes.
About Mayo Clinic
Mayo Clinic is a nonprofit worldwide leader in medical care, research and education for people from all walks of life. For more information, visit mayoclinic.com and mayoclinic.org/news.
###
MEDIA CONTACT: Kevin Punsky, Mayo Clinic Public Affairs, 904-953-0746.
Email: punsky.kevin@mayo.edu







