-
Health & Wellness
Mayo Clinic Q and A: Lifestyle changes often help ease symptoms of peripheral artery disease
 DEAR MAYO CLINIC: My mother, 67, was recently diagnosed with peripheral artery disease. She has been having leg pain and other symptoms for many months. She was prescribed medication but her doctor said she may need surgery. What would that involve? Are there any other treatment choices?
DEAR MAYO CLINIC: My mother, 67, was recently diagnosed with peripheral artery disease. She has been having leg pain and other symptoms for many months. She was prescribed medication but her doctor said she may need surgery. What would that involve? Are there any other treatment choices?
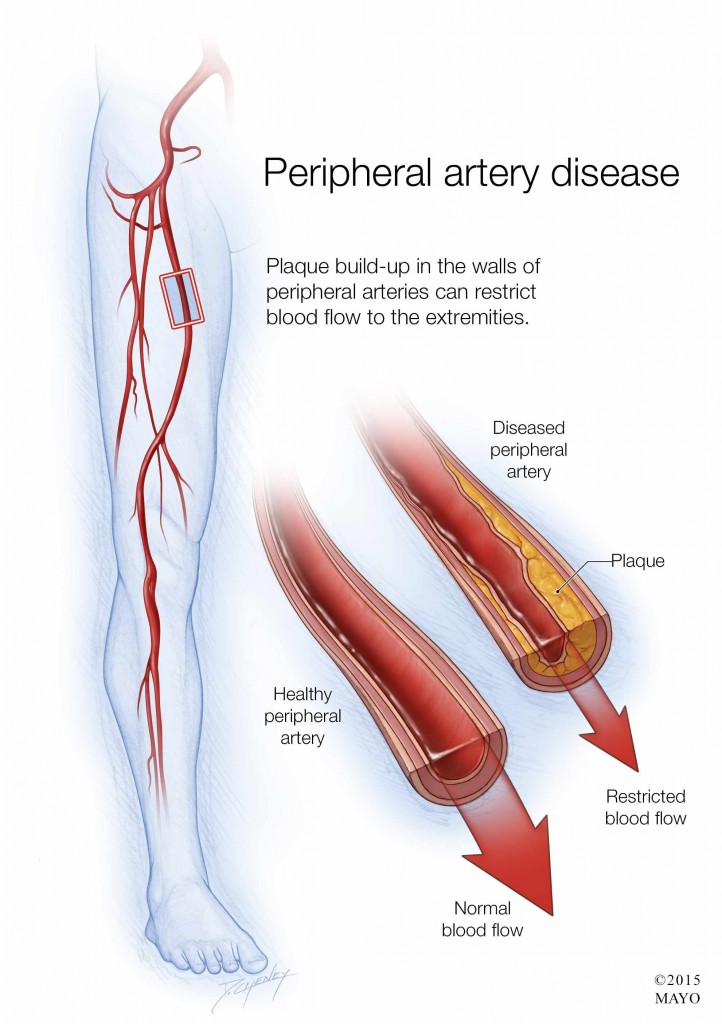
ANSWER: In people who have peripheral artery disease, narrowed arteries limit blood flow to the arms and legs. When the limbs do not get enough blood, it can trigger a variety of symptoms. The most common include leg pain when walking, leg cramps after doing an activity, leg numbness and leg weakness. If left untreated, pain and other symptoms may get worse over time.
Treatment for peripheral artery disease usually includes lifestyle changes and medication. For many people, those two therapies are all they need to effectively manage the disease. If they are not enough, though, a procedure to open blocked arteries (angioplasty) may be recommended. Surgery to bypass a blocked or narrowed artery can be another useful treatment option for some cases of peripheral artery disease.
Lifestyle changes often can help ease symptoms and slow the disease’s progress. Smoking is one of the biggest risk factors for peripheral artery disease. Smoking frequently leads to artery narrowing and damage. It also can make the disease get worse more quickly. If your mother smokes, quitting is one of the most important steps she can take to combat peripheral artery disease.
Exercise, usually in the form of a walking program, also can help. In many cases, walking 30 minutes a day at least three times a week conditions muscles to more efficiently use the oxygen they get from the blood. That can lessen the pain and other symptoms, allowing people with this disease to walk farther distances. If she has not already done so, suggest that your mother talk with her doctor about creating an exercise plan that fits her needs.
Medication may reduce symptoms, too. For example, drugs such as cilostazol and pentoxifylline can help improve blood flow and widen blood vessels. Aspirin therapy is often used to prevent blood clots in people with peripheral artery disease. In addition, medications to control other health conditions that contribute to peripheral artery disease (such as high blood pressure, diabetes and high cholesterol) are often recommended.
If lifestyle changes and medication do not improve the symptoms of peripheral artery disease, then angioplasty might be a good option. During this procedure, a doctor threads a small tube called a catheter through a blood vessel to the narrowed artery. A small balloon on the tip of the catheter is inflated to flatten the blockage into the artery wall and stretch the artery open to increase blood flow. The doctor may also insert a mesh framework called a stent in the artery to keep it open. Angioplasty typically is an outpatient procedure that does not require an overnight hospital stay.
In certain situations including complete blockage of the artery, unsuccessful angioplasty, or if a stent is not appropriate, bypass surgery may be recommended. During bypass surgery, a surgeon removes a blood vessel from another part of the body, or uses an artificial blood vessel, in order to direct blood around the blocked artery. Results of bypass surgery usually last longer than angioplasty, but it is a more invasive procedure that requires a hospital stay and involves a longer recovery.
The treatment choice your mother makes likely will be based on the severity of her peripheral artery disease and where the blocked arteries are located, as well as her personal preferences and other medical conditions she may have. Encourage her to review all her options with her physician and discuss the risks and benefits of each before she makes a decision. — Randall De Martino, M.D., Vascular Surgery, Mayo Clinic, Rochester, Minn.
Related Articles







