-
Mayo Clinic Q and A: How to manage symptoms of liver disease
DEAR MAYO CLINIC: My husband is 45 and has lived with irritable bowel syndrome for many years. He was recently diagnosed with primary sclerosing cholangitis. Are these two conditions related? We were told a liver transplant was likely in the future. Do all people require a transplant? Are other treatments available to manage this liver disease?
ANSWER: Primary sclerosing cholangitis is not associated with irritable bowel syndrome, but it can be related to another condition broadly termed inflammatory bowel disease, or more specifically ulcerative colitis. Your husband should be tested for ulcerative colitis if this testing has not already occurred.
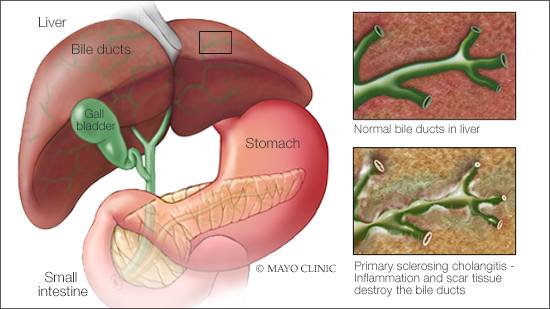
Primary sclerosing cholangitis is a rare disease that affects the ducts that carry the digestive liquid bile from your liver to your small intestine. In people who have primary sclerosing cholangitis, inflammation causes scars within the bile ducts. The scars make the ducts hard and narrow. Over time, this can cause serious liver damage.
While many people who have primary sclerosing cholangitis eventually need a liver transplant, that is not the case for everyone. Regular monitoring and follow-up care can manage symptoms and identify complications of primary sclerosing cholangitis early.
Primary sclerosing cholangitis often progresses slowly. As it advances, the disease may result in repeated infections, and can lead to bile duct tumors or liver tumors. Eventually, primary sclerosing cholangitis may cause the liver to fail.
On average, it takes about 10 years until most people with primary sclerosing cholangitis need a liver transplant. However, the rate at which primary sclerosing cholangitis progresses varies widely. Some people with this disease live a normal life span without ever progressing to liver failure or needing a transplant.
To manage care going forward, your husband should work with a hepatologist, which is a physician who specializes in liver disorders. Based on a number of laboratory and clinical factors, the hepatologist can help your husband calculate the risk for liver failure and coordinate the ongoing monitoring needed.
It also would be valuable to talk with the hepatologist about scheduling a colonoscopy, especially if your husband has not had one. This examination would help determine if underlying ulcerative colitis is an issue. Random biopsies of tissue in the colon are recommended, even if the mucosa appears normal, since ulcerative colitis in people with primary sclerosing cholangitis may be mild at first and may not be apparent without tissue specimens.
In addition to monitoring your husband's condition, a hepatologist also can manage symptoms and complications of primary sclerosing cholangitis, such as fatigue, itching and infections.
If possible, consider consulting with a hepatologist at an academic medical center with a strong hepatology division. Specialists at these centers can offer your family the most up-to-date care. In addition, these centers often have access to research trials that focus on new treatment options.
Although no specific medical therapy is approved for primary sclerosing cholangitis, a number of research trials studying primary sclerosing cholangitis treatment are underway and more are coming soon. These trials can be an excellent way for people who have primary sclerosing cholangitis to get treatment they may benefit from years before those agents are approved by the Food and Drug Administration.
At this time, a liver transplant is the only treatment known to cure primary sclerosing cholangitis. Liver transplant generally is reserved for people with liver failure or other severe primary sclerosing cholangitis complications. While uncommon, it is possible for primary sclerosing cholangitis to return, even after a liver transplant. — Dr. Elizabeth Carey, Transplant Hepatology, Mayo Clinic, Phoenix
****************************
Related Articles
- Adopted boy thriving after liver transplant published 4/20/22
- Mayo Clinic Minute: ‘Liver in a box’ is saving lives with new technology published 4/18/22
- Science Saturday: Regenerative technology uncovers new discoveries in liver disease published 11/20/21
- Mayo Clinic Q&A podcast: Reducing rejection by reversing order of heart-liver transplant published 4/27/21
- Reverse-order heart-liver transplant helps prevent rejection for highly sensitized patients published 4/1/21
- College athlete undergoes liver transplant while infected with COVID-19 published 2/10/21
Related Articles







